Developing a blended learning orientation programme for junior doctors in Neonatology
Submitted: 19 October 2023
Accepted: 25 March 2024
Published online: 2 July, TAPS 2024, 9(3), 58-60
https://doi.org/10.29060/TAPS.2024-9-3/CS3159
Wing Yee Tong1, Bin Huey Quek1, Arif Tyebally2 & Cristelle Chow3
1Department of Neonatology, KK Women and Children’s Hospital, Singapore; 2Emergency Medicine, KK Women and Children’s Hospital, Singapore; 3Department of Paediatrics, KK Women and Children’s Hospital, Singapore
I. INTRODUCTION
Neonatology is considered a ‘niche’ paediatric subspecialty. Most junior doctors posted to the department have limited prior exposure to the neonatal population, and require quick and effective training to help them function safely on the clinical floor. In recent years, postgraduate medical teaching has found the use of blended learning to be effective (Liu et al., 2016). Blended learning is defined as a combination of classroom face-time with online teaching approaches, and there is currently paucity of literature on its efficacy in ‘up-skilling’ relatively inexperienced healthcare professionals in a subspecialty setting. Hence, the aim of this study was to design and evaluate the efficacy of a blended-learning orientation programme in improving neonatal clinical knowledge and procedural skills amongst junior doctors.
II. METHODS
A. Study Setting and Participants
This study was set in the largest academic tertiary paediatric hospital in Singapore.
B. Curriculum Development
We adopted the Kern’s six-step approach for curriculum development (Thomas et al., 2022), as it systematically identifies and addresses learner needs, and its cyclical nature also allows for constant modifications and improvements.
1) Step 1: Problem identification and general needs assessment
We conducted a quantitative survey to identify the general issues with our current programme, which consisted of daily face-to-face, largely didactic lectures over the first month of the posting. We noticed that many junior doctors missed teaching sessions due to work obligations, resulting in ‘piecemeal’ and ineffective learning. The one-month programme was also considered excessively lengthy.
2) Step 2: Targeted needs assessment
Most junior doctors considered themselves to be ‘novice’ learners in neonatology. This emphasised the importance of starting with foundational teaching concepts to avoid overwhelming them. Junior doctors also preferred interactive learning methods.
3) Step 3: Goals and objectives
Our main objective was for the junior doctors to be competent and safe members of the clinical team, with basic neonatal clinical knowledge and the ability to perform and assist in neonatal procedures.
4) Step 4: Educational strategies: Course content development
We identified a list of core topics and procedural skills which formed the programme curriculum (Figure 1).
The teaching format was changed from mainly didactic lectures to case-based scenarios in both online and face-to-face sessions, as this has been shown to better motivate students towards self-directed learning and develop problem-solving skills. Case-based scenarios would also facilitate greater peer discussion and interactivity amongst learners in the face-to-face sessions.
We worked with IT specialists to convert specific topics to six online learning modules, and included interactive components such as clickable elements and narration to better engage learners (Choules, 2007). Each module was designed to be completed within 30 minutes.
For neonatal procedural skills, learners were expected to watch online demonstration videos created by the department prior to attending hands-on practical sessions.
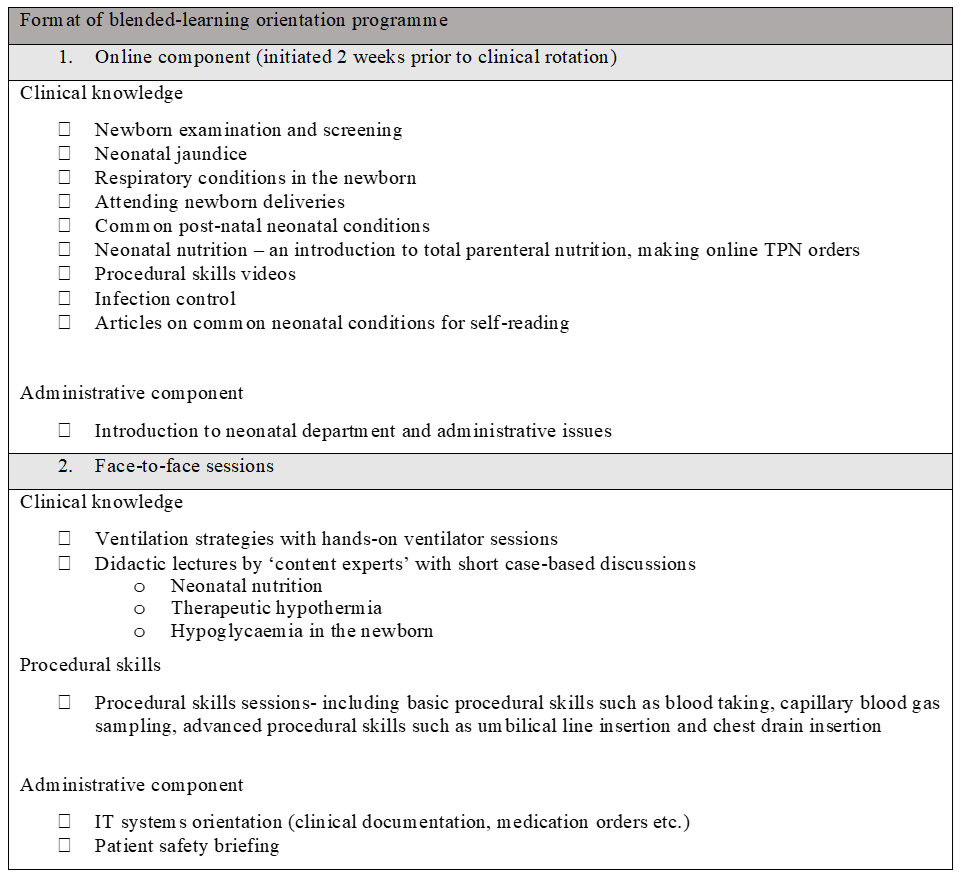
Figure 1. Outline of blended-learning orientation programme
5) Step 5: Implementation
The blended learning programme was implemented with junior doctors across two batches from July 2022 to January 2023. Majority were from post-graduate year three to five, with approximately half having no prior working experience in neonatology. All participated in the face-to-face sessions and completed the online modules.
We used our institution’s online learning management system to deliver the e-learning modules, and department faculty members conducted the face-to-face sessions. Designated ‘protected teaching time’ was implemented to facilitate attendance during office hours.
6) Step 6: Evaluation and feedback
We designed a pre-and-post-programme assessment consisting of 24 multiple-choice questions covering the following aspects – (1) clinical scenarios with interpretation of laboratory and radiological results, (2) factual knowledge and (3) questions on procedural skills.
The junior doctors also completed an online survey which assessed the learners’ perceptions on blended learning. Consent for the survey data to be used for research was implied in their participation.
III. RESULTS
The junior doctors had a positive experience with blended learning. All participants agreed that the learning content was relevant and appropriate for their level of experience. Almost all participants felt that there was ease of access to the online learning modules, with minimal technical issues. Learners also found specific online modules such as respiratory conditions ‘useful’, but enjoyed the face-to-face nature of sessions such as ventilatory strategies, as it gave them the opportunity to clarify doubts with their facilitator. Overall, the duration of the face-to-face orientation sessions was halved, and there was a significant improvement in the mean MCQ score.
IV. DISCUSSION
A blended learning programme designed for novice learners in Neonatology is effective in preparing junior doctors for clinical work.
Learning theories suggest that adult learners are motivated to invest time in learning if they understand its relevance (Taylor & Hamdy, 2013). The shift towards case-based learning bridges theory and practice, and motivates participation in clinical decision-making. This is an effective form of learning as demonstrated by an improvement in the mean post-test MCQ score of the participants. The experience was also deemed a positive one in qualitative feedback. In addition, the accessibility of online modules provided learners with autonomy to control their pace of learning. However, it is important to strike the right balance between online and classroom teaching, as learners still value the interactivity offered by face-to-face teaching.
We should work to create a supportive infrastructure to support blended learning methods by training more clinician-educators in online learning approaches and designing ‘reusable’ learning resources, which can be modified and integrated into other medical courses in future (Singh et al., 2021).
The limitations of our study include reliance on multiple choice tests to assess knowledge, and a lack of formal evaluation of procedural skills. Competency-based evaluations, as well as practical skills evaluations can be implemented in future runs to evaluate the efficacy of the courses.
V. CONCLUSION
Technology enhanced learning is fast becoming an integral part of medical education. Through this study, we demonstrate that blended learning programmes can be successfully integrated into the training of junior doctors in a subspecialty setting.
Notes on Contributors
WT led the design and conceptualisation of this work, implemented the education programme, and drafted the manuscript. BQ provided feedback and guidance on creating the content of the education programme. CC provided guidance on the evaluation of teaching programme. CC, AT and BQ provided feedback on the manuscript. All authors approve the publishing of this manuscript.
Funding
The authors received a Singhealth Duke-NUS Academic Medicine Education Institute Education Grant 2021 (funding number EING2205) to support the development of curriculum content for our programme.
Declaration of Interest
All authors declare that there are no conflicts of interest.
References
Choules, A. P. (2007). The use of elearning in medical education: A review of the current situation. Postgraduate Medical Journal, 83(978), 212-216. https://doi.org/10.1136/pgmj.2006.05 4189
Liu, Q., Peng, W., Zhang, F., Hu, R., Li, Y., & Yan, W. (2016). The effectiveness of blended learning in health professions: Systematic review and meta-analysis. Journal of Medical Internet Research, 18(1), e2.
Singh, J., Steele, K., & Singh, L. (2021). Combining the best of online and face-to-face learning: Hybrid and blended learning approach for COVID-19, post vaccine, & post-pandemic world. Journal of Educational Technology Systems, 50(2), 140-171. https://doi.org/10.1177/00472395211047865
Taylor, D. C., & Hamdy, H. (2013). Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83. Medical Teacher, 35(11), e1561-e1572. https://doi.org/10.3109/0142159x.2013.828153
Thomas, P. A., Kern, D. E., Hughes, M. T., Tackett, S. A., & Chen, B. Y. (Eds.). (2022). Curriculum development for medical education: A six-step approach. Johns Hopkins University Press.
*Tong Wing Yee
100 Bukit Timah Road
Singapore 229899
Email: tong.wing.yee@singhealth.com.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









