What dress code do we teach students and residents? A survey of patients’ and their families’ preferences regarding physicians’ appearance
Submitted: 1 September 2023
Accepted: 29 January 2024
Published online: 2 July, TAPS 2024, 9(3), 32-40
https://doi.org/10.29060/TAPS.2024-9-3/OA3127
Michiko Goto1, Ryota Sakamoto2, Hideki Wakabayashi3 & Yousuke Takemura4
1Department of General Medicine, Mie University School of Medicine, Japan; 2Department of Medical Informatics, Mie University Hospital, Japan; 3Department of Community Medicine, Mie University School of Medicine, Japan; 4Department of General Medicine, Tokyo Women’s Medical University, Japan
Abstract
Introduction: From the late 1960s to the present, physicians’ dress codes have been actively studied in Western countries. Until the early 21st century, patients tended to prefer a conservative dress style, such as “shirt and tie or skirt” with white coats for physicians. However, as attitudes toward dress codes have changed, knowledge regarding this issue needs to be updated. A variety of colours of scrubs are currently commonly used by medical professionals, but it is not known whether all colours are acceptable to patients. The current study sought to investigate the acceptability of various dress codes for physicians from the patients’ perspective, to inform medical education.
Methods: Outpatients and their family members at a university hospital and a small-to-medium-sized hospital were surveyed. We inquired about which of the different styles of white coats and different colours of scrubs were most desirable for male and female physicians. We used Scheffe’s paired comparison method to determine rankings.
Results: Patients and their family members expected their physicians to wear white coats rather than scrubs. Furthermore, a more traditional and formal dress code was preferred. The least preferred colour of scrubs was yellow.
Conclusion: The current results indicated that patients’ preference for a traditional, conservative appearance has not changed over time. This finding does not match current perspectives on infection prevention. Both patient preferences and infection prevention are important for informing education and gaining patient trust.
Keywords: White Coat, Scrub Colour, Physicians’ Appearance, Medical Education, Doctor-Patient Communication
Practice Highlights
- The physician’s traditional white coat may be associated with a sense of trust, and is most preferred by patients and their family members. This trend has not changed over time.
- Among the scrub colours, bright colours are not preferred, and black and red may have a negative meaning for patients and their family members.
- Regarding dress code education, patient/family perspectives, infection prevention, and sociocultural background should all be considered.
I. INTRODUCTION
Hippocrates proposed that physicians should “be clean in person, well dressed, and anointed with sweet smelling unguents” (Hippocrates, 1923). However, it has not been proven that physicians’ appearance affects their competence or patients’ satisfaction (Hennessy et al., 1993; Neinstein et al., 1985; Takemura et al., 2008). Nevertheless, some researchers have reported that a physician’s appearance is “important” (Brandt, 2003) as a surrogate for proof of physicians’ competence among unfamiliar patients (Jacob, 2007), and others have given credence to this notion (Baxter et al., 2010). While the white coat is considered to be a symbol of power and authority (Bond et al., 2010), it has also been reported to be a sign of trust and credibility (Brandt, 2003; Gherardi et al., 2009; Nair et al., 2002; Rehman et al., 2005). Additionally, an unkempt appearance may be interpreted as reflecting a lack of skill and care (Gjerdingen et al., 1987).
As lifestyles have changed with the development of new materials, attitudes toward clothing have also changed. However, patients’ viewpoints regarding physicians’ clothing have not been evaluated since the end of the “formal dress: shirt and tie” era (Toquero et al., 2011). Therefore, there is a need to conduct dress code surveys to update current knowledge regarding the consequences of these changes. From the late 1960s to the present, dress codes have been actively studied in the West (Blumhagen, 1979; Gledhill et al., 1997; Menahem & Shvaretzman, 1998). Studies conducted at the beginning of the 21st century reported that patients tended to prefer physicians wearing white coats over formal attire (Keenum et al., 2003; Nair et al., 2002). In Japan, there have been very few studies of physicians’ dress codes (Ikusaka et al., 1999; Yamada et al., 2010). However, in a survey of more than 2,000 patients, Yamada et al. (2010) reported that white coats and ties worn by male physicians and knee-length skirts and white coats worn by female physicians were the dress codes considered most acceptable by patients.
The outbreak of severe acute respiratory syndrome mainly in Canada and Asian countries east of India substantially changed the medical environment and the dress code for physicians (Au-Yeung, 2005). The “scrub,” a surgical garment that can be easily worn in medical settings, is used by many healthcare professionals as daily medical clothing, and its use has continued to increase even after the severe acute respiratory syndrome epidemic ended, thus making scrubs an important focus of dress code research (Gherardi et al., 2009). The bare below the elbows (BBE) policy specifies that sleeves should be rolled up to avoid infection, and research has been conducted to determine the extent to which patients are willing to accept this attire (Aitken et al., 2014; Bond et al., 2010). In 2005, Japan’s Ministry of the Environment promoted the Cool Biz initiative, which encourages workplaces to use “appropriate room temperature settings and encourage employees to wear light clothing appropriate to those temperatures during the summer months” (Ministry of the Environment, 2017). In 2011, as these changes began to spread among the general public, the Great East Japan Earthquake occurred, resulting in the Fukushima power plant meltdown. Emergency national energy-saving measures were implemented, which accelerated the adoption of the Cool Biz approach. The concept of Cool Biz, as promoted by the Japan government, spread rapidly, with several surveys reporting a sharp decline in the wearing of ties in offices (Nishihara et al., 2010; Nishina et al., 2007). Many hospital directors of medical institutions asked patients to accept their staff wearing light clothing during the summer, such as dressing without neckties; thus, we assume that dressing without a tie also became widespread in medical settings (Keio University Hospital, 2014). We speculate that the number of physicians who dress formally was reduced following this trend. Moreover, although no systematic evidence has been reported, as noted in a study by Kurihara et al. (2014), more doctors began to wear scrubs and Crocs-style shoes, possibly because of the influence of American TV dramas and medical films.
As a result, these changes in the environment led to confusion in medical education, with different teachers providing different dress instructions, and students having difficulty understanding the rationale for teachers’ dress instructions.
The aim of the current study was to investigate the acceptability of dress codes from the patients’ perspectives, and to inform medical education. The findings of this study may be useful for medical teachers, doctors, and medical institutions as a reference when instructing medical students and doctors regarding how to choose clothing.
II. METHODS
Convenience sampling was conducted among outpatients and their family members while they were waiting for treatment at two medical institutions: a university hospital with 655 beds in a central area of Tsu city, and a primary care centre with 82 beds in a rural area on the outskirts of Tsu city, Japan. Tsu has a population of 270,000 people, and is located 400 km south-west of Tokyo. The main industries in the city are the manufacturing of transport machinery, information and communication equipment, and foodstuffs, but there are also many agricultural workers in the surrounding area, making it a typical regional city in Japan in many respects. The study period was 3 years, from April 2012 to August 2015. The subjects were asked about their sex, age, and the department in which they were treated. The surveyed items included various styles of dress mentioned in previous studies (formal, casual, and scrubs) and variations in wearing practices that have been observed in the field (open-front white coats, masks, slippers, rolled-up sleeves, Casey [A short white coat with a closed front] short sleeves, and open-front scrubs). This ultimately resulted in nine different styles for men and seven different styles for women (excluding ties and Casey short sleeves). Moreover, 15 different colours of scrubs were selected to cover most of the available colours ones on the market (Figure 1) for a survey on undesirable colours for physician’s wear.
A. Survey
For Question 1, participants were asked to compare pictures of two doctors and to choose one of four levels of response (completely A, more like A, or more like B, completely B). Participants were instructed to choose one of them, even if it was difficult to decide.
Images of nine different types of attire for male physicians and seven different types of attire for female physicians were prepared, in mature and younger versions. The nine types of attire for men were as follows: ① tie + white coat with front closed, ② tie + white coat with front open, ③ white coat with no tie, ④ slippers, ⑤ mask, ⑥ Casey, ⑦ rolled-up sleeves, ⑧ scrubs + white coat, and ⑨ scrubs. The seven types for women were as follows: ① white coat with front closed, ② white coat with front open, ③ rolled-up sleeves, ④ sandals, ⑤ mask, ⑥ scrubs + white coat, and ⑦ scrubs.
Nine photos of men in pairs (one adult version and one young version) were presented in a round-robin fashion on an iPad. Seven photos of pairs of women (one adult version and one young version) were shown in the same way. Patients and their family members were asked to compare the two photos and to select the one that they felt was more appropriate as their physician’s appearance, using four levels of response. We also asked participants to identify any images showing an “unacceptable appearance.”
For Question 2, patients were instructed to identify any colours that they felt were not desirable for a doctor to wear. The commercially available colours used were a mix of cold and warm colours. Fifteen images of scrubs (black, grey, light blue, light purple, dark blue, blue-green, dark blue-green, dark green, yellow, orange, brown, pink, dark pink, red, and red-purple) were shown on an iPad to the subjects, who were then asked to indicate any unacceptable colours (Figure 1).

Figure 1. Scrubs in 15 different colours
1: black, 2: grey, 3: light blue, 4: light purple, 5: dark blue, 6: blue-green, 7: dark blue-green, 8: dark green, 9: yellow, 10: orange, 11: brown, 12: pink, 13: dark pink, 14: red, 15: red-purple
B. Statistical analysis
For Question 1, we used Scheffe’s paired comparison method (Nakaya’s variant) to rank data as completely A +2, more like A +1; unanswered/invalid 0, more like B −1; and completely B −2, as fitted. A one-way analysis of variance was performed within subjects.
III. RESULTS
We received 869 responses regarding the appearance of young men and women, 824 responses regarding the appearance of mature men and women, and 867 responses regarding unacceptable scrub colours.
A. Question 1
1) Young men: The descending order of preference for young men was as follows: ① tie + white coat, ⑥ Casey, ⑦ rolled-up sleeves, ③ no tie + white coat, ② tie + open-front white coat, ④ slippers, ⑧ scrubs + white coat, ⑤ mask, and ⑨ scrubs (Figure 2). Clearly, ④ slippers and below constituted the subgroups, and there was no significant difference between ⑤ mask and ⑨ scrubs (Figure 2).
A total of 300 individuals reported 427 images showing unacceptable appearances, of which 42% showed the physician wearing scrubs (Table 1).
2) Mature men: The descending order of preference for mature men was as follows: ① tie + white coat, ⑥ Casey, ② tie + white coat with front opening, ③ no tie + white coat, ⑦ rolled-up sleeves, ④ slippers, ⑤ mask, ⑨ scrubs, and ⑧ scrubs + white coat. As in the case of the young men, ④ slippers and below constituted a lower group, and there was no significant difference between ⑨ scrubs and ⑧ scrubs + white coat (Figure 2).
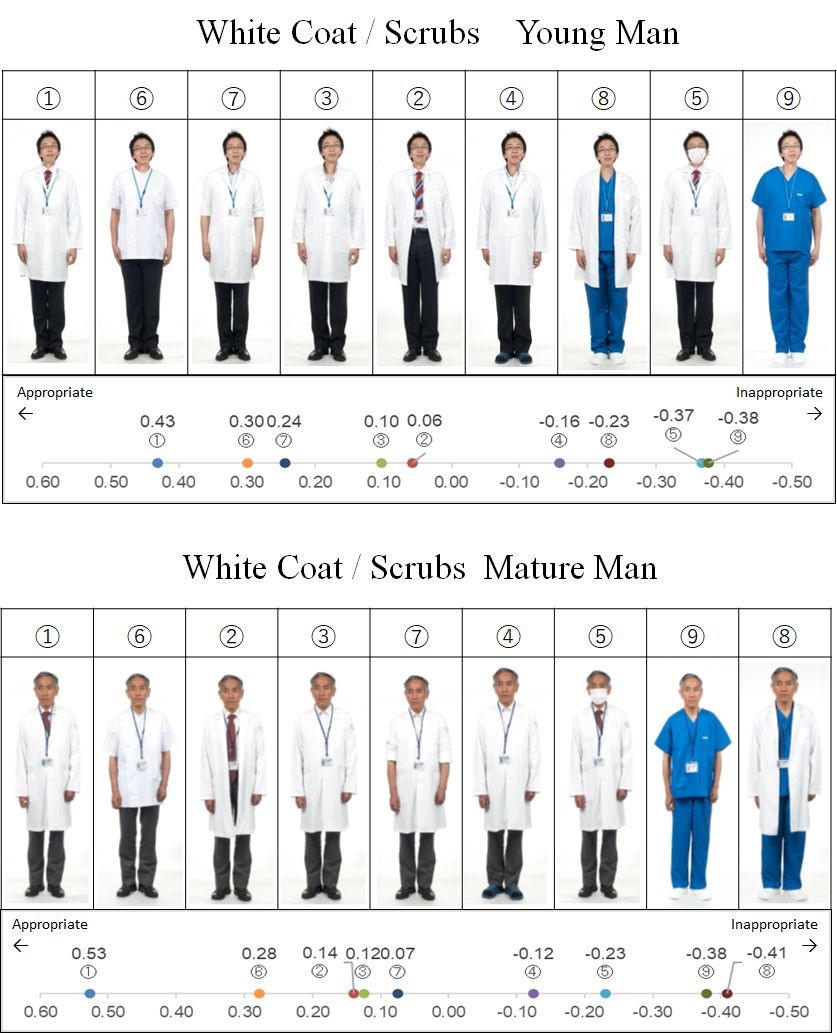
Figure 2. Nine types of attire for mature and young male physicians, each in order of patient preference with scale chart of average degree of preference
*The yard stick values were Y0.05=0.052 for young men and 0.054 for mature men
A total of 264 individuals reported 354 images showing unacceptable appearances, of which 40% showed the physician wearing scrubs (Table 1).
3) Young women: The descending order of preference for images of young women was as follows: ① white coat, ③ sandals, ② open-front white coat, ④ mask, ⑤ rolled-up sleeves, ⑥ scrubs + white coat, and ⑦ scrubs (Figure 3). Moreover, ① white coat and ③ sandals formed the top group; ② open-front white coat and ④ mask formed the middle group; and ⑤ rolled-up sleeves, ⑥ scrubs + white coat and ⑦ scrubs formed the lower group. There were no significant differences between the groups (Figure 3).
A total of 403 individuals reported 535 images showing unacceptable appearances, of which 57% featured rolled-up sleeves and 33% featured scrubs (Table 1).
|
Physician’s Appearances |
Young man n = 300 |
Mature man n = 403 |
Young woman n = 264 |
Mature woman n = 172 |
|
Tie + white coat |
0% |
2% |
|
|
|
No tie + white coat |
5% |
7% |
|
|
|
White coat |
|
|
2% |
1% |
|
Tie + open-front white coat |
18% |
17% |
|
|
|
Open-front white coat |
|
|
8% |
16% |
|
Slippers |
20% |
9% |
18% |
23% |
|
Mask |
28% |
20% |
2% |
2% |
|
Casey |
3% |
4% |
|
|
|
Rolled-up sleeves |
5% |
9% |
57% |
15% |
|
Scrub + white coat |
21% |
26% |
12% |
25% |
|
Scrub |
42% |
40% |
33% |
48% |
Table 1. The characteristics of images that were identified as showing an unacceptable appearance by patients and their family members, and the percentage of respondents that deemed the image unacceptable
4) Mature women: The descending order of preference for images of mature women was as follows: ① white coat, ③ sandals, ④ mask, ② open-front white coat, ⑦ scrubs, ⑤ rolled-up sleeves, and ⑥ scrubs + white coat (Figure 3). There was no significant difference between the components ① white coat and ③ sandals in the top group. Moreover, ① white coat and ③ sandals were components of the top group, similar to the case for images of young women, and there was no significant difference between them (Figure 3).
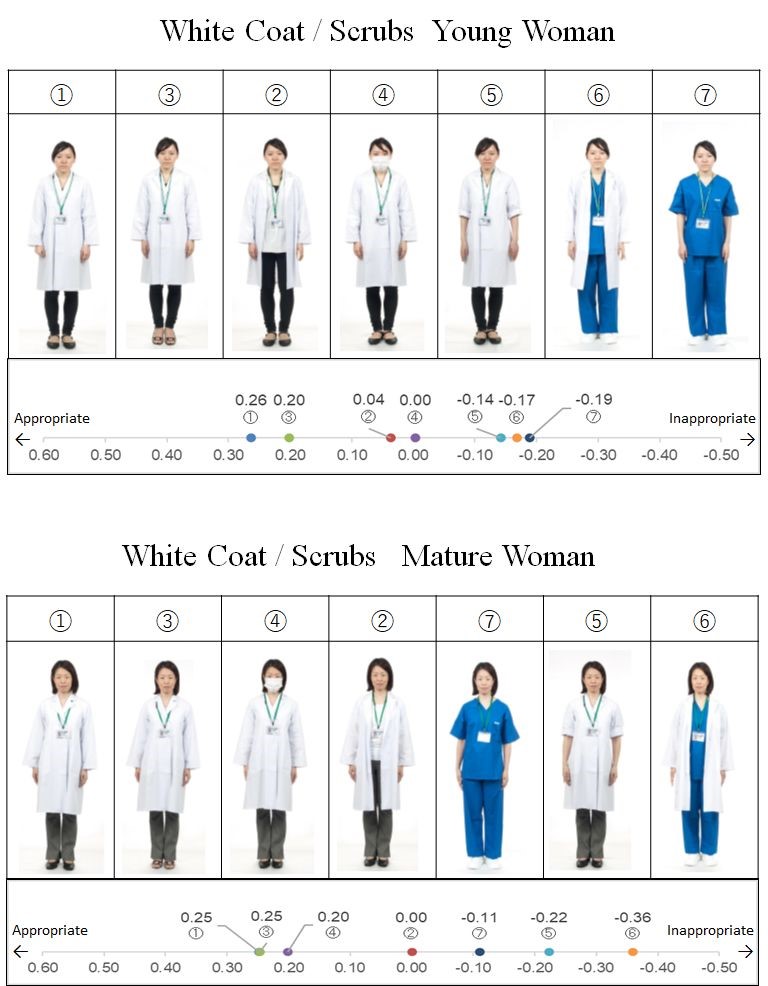
Figure 3. Seven types of attire for mature and young female physicians, each in order of patient preference with scale chart of average preference
*The yard stick values are Y0.05=0.054 for young women and 0.061 for mature women
A total of 172 individuals reported 222 images showing unacceptable appearances, of which 48% featured scrubs (Table 1).
We examined the trends by participants’ gender and age. The results revealed no differences between men and women and in each age group. However, participants over 70 years old tended to prefer tie + closed- and open-front white coat compared with participants under 70, and tended not to favour female doctors with rolled-up sleeves.
B. Question 2
1) Scrub colour: The colours and percentages of scrubs that were identified as unacceptable were, in descending order, as follows: 52%, yellow; 46%, red; 42%, dark pink; 33%, pink; 27%, black; 23%, orange; 20%, blue-green; 16%, grey; 17%, red-purple; 14% brown; 11%, dark blue-green; 8%, light blue; 7%, dark green; 6%, light purple; and 4%, dark blue (Figure 4).

Figure 4. Percentage of scrub colours not preferred by patients and their family members.
IV. DISCUSSION
Many patients and their family members expected their physicians to wear white coats rather than scrubs. On average, a traditional and formal dress style was most preferred by patients and their family members (buttoned white coat and tie for men, leather shoes, and buttoned white coat for women). In a 2010 study conducted in Japan by Yamada et al., the most favoured formality attire by patients was white coats (but skirts for women). Pronchik, who investigated the benefits of neckties prior to the BBE policy (King & Infection Prevention and Control Nurse, 2022), concluded that in an emergency room in the United States (US), patients preferred their physicians to wear ties, and patient satisfaction was high (Pronchik et al., 1998). The survey found that people in older age groups in particular preferred doctors to wear ties.
The results suggest that patients’ preferences regarding physicians’ appearance have not changed substantially. One study found that patients in the United Kingdom (UK) who were briefed on the BBE policy felt that conservatively dressed doctors looked more professional (Toquero et al., 2011).
The second-most preferred attire for male physicians was the Casey, followed by the white coat with rolled-up sleeves for younger men. However, this attire was not ranked highly for women or mature men. This indicates that patients perceived the Casey as a traditional style of dress for men, and that the preference was not necessarily based on the prevalence of the BBE concept or concerns about cleanliness. The pros and cons of rolling up the sleeves of white coats are often discussed in medical student dress guidance, including in a study by Bond (Bond et al., 2010). In the current study, rolled-up sleeves were not preferred by patients. However, it is known that the sleeves of white coats can become contaminated (Banu et al., 2012), and Wong et al. pointed out that the risk of contamination may be increased by pathogens in ties, cuffs, and pockets (Wong et al., 1991). The current results indicated that patients in their 70s and older were not comfortable with female doctors rolling up the sleeves of their white coats. Although this finding may be related to cultural factors, to the best of our knowledge, this phenomenon has not been previously reported in the literature. The results suggest that patients’ concepts of professionalism and infection prevention are not directly connected. When instructing students about dress code, they should be told that patients may not approve of rolling up their sleeves.
Men wearing masks were rated less favourably, while women wearing masks were not rated less favourably. For women, there may be something to compensate for the facial expressions hidden by masks. Because wearing a mask and other prophylactic devices has been essential for physicians since the beginning of the COVID-19 pandemic, the impressions of patients and family members should be examined in future studies.
Although scrubs are often rated as hygienic (Bond et al., 2010; Lightbody & Wilkie, 2013), the current survey revealed that scrubs were not rated as a preferred attire for physicians by patients and their family members. In the survey by Aitkin et al. mentioned above, scrubs also received the lowest ratings. However, previous studies in the US reported no influence of scrubs and other types of attire on patient satisfaction and perceptions of professionalism (Fischer et al., 2007; Li & Haber, 2005). Additionally, a recent survey in the UK reported a clear downward trend in resistance to scrubs, with a survey by Palazzo and Hocken reporting that white coats and ties are no longer expected by patients (Palazzo & Hocken, 2010). In a study in the US, patients undergoing surgery reported that scrubs were most favoured in outpatient settings (Edwards et al., 2012). These findings suggest that the resistance to scrubs in Japan may disappear in the near future.
Brightly coloured (yellow, red, and pink) and black scrubs were considered to be less acceptable than others, and those in pale and cold colours, such as dark blue and light blue, were preferred. This may have occurred because red and black are associated with negative emotions such as anger, anxiety and fear, whereas cold colours are associated with calm and quiet (Oyama et al., 1963). Some patients commented that black reminded them of death and red reminded them of blood. Bright colours may be irritating to patients. To the best of our knowledge, no previous studies have examined colour preferences for scrubs among patients, suggesting that these findings are novel.
In the 20th century, physicians in many countries were required to wear white coats (Gooden et al., 2001; Harnette, 2001). It is not surprising that preferences regarding physicians’ appearance have changed in the 21st century, as many people have started to become more familiar with the threat of infection and changes in the global medical environment. However, the concept of BBE is still not pervasive, and the appearance of attire required to be worn by physicians has not changed significantly. The current results are consistent with the findings of the largest study of this issue conducted in the UK (Jacob, 2007), which reported the following: “if there is deemed to be no significant infection risk from any given variation of workwear, our patients would like us to wear a shirt and tie.” Patients’ awareness regarding infection needs to be investigated, but patients will accept physicians’ suggestions if they understand the need for them (Collins et al., 2013).
Shelton et al. conducted an experiment in the UK to reduce cross-infection between doctors and patients, and reported that there was no significant difference in patient preferences between different types of attire before explaining the importance of clothing to patients; however, after the explanation, scrubs and short-sleeved shirts were most preferred (Shelton et al., 2010). When considering physicians’ dress code, we need to understand both the patient’s preferences and infection control factors. We propose that a dress code should be developed that does not compromise patients’ trust and confidence, but also takes safety into consideration.
A. Limitations
Although the types of clothing shown in the photos in the current study were based on a prior survey, it may not have been comprehensive. Moreover, using different models in the photographs may have influenced the results, and the potential effects of measurement bias cannot be excluded. It is unclear from the current findings why certain appearances were preferred or deemed unacceptable. Furthermore, the current study did not examine doctors’ preferences. Medical practitioners’ preferences need to be taken into account when making workplace attire choices in hospitals. Further research will be needed to identify the preferred attire for both patients and doctors.
V. CONCLUSION
The current findings indicated that patients exhibited a preference for physicians dressed in traditional attire. Even though times have changed, people may still associate trust, credibility, and respect with the formal appearance of their physicians. The current findings also suggested that patients were not aware of the BBE policy. The results of this study may be helpful for informing teaching approaches regarding the appearance of medical students and residents.
Notes on Contributors
MG developed the research idea and design with YT. The data collection was performed by MG. The data were analysed by RS. HW performed the data interpretation with MG. MG wrote the article with revision by HW. All the authors read and agreed with the final manuscript.
Ethical Approval
Verbal informed consent was obtained from all participants for publication and this procedure was approved by the Mie University Ethics Committee. The Ethical Review Committee of Mie University committee approved this study (No. 1237). All methods were performed in accordance with the relevant guidelines and regulations.
Data Availability
The data that support the findings of this RCT study are openly available at a Figshare repository, https://doi.org/10.6084/m9.figshare.23936379.v1
Acknowledgements
We would like to express our heartfelt gratitude to the models for their cooperation in creating the photograph stimuli, and to Goto F, Makita H, Yin M, Kasyo K, Sakaguchi R, Masukawa E, Tsunoda K, Shimada K, and Tanaka K, for collecting the data. We thank Benjamin Knight, MSc., from Edanz (https://edanz.com) for editing a draft of this manuscript. This paper has been preprinted. M Goto et al. What dress code do we teach students and residents? A survey of patients’ and their families’ preferences regarding physicians’ appearance. 23 Mar, 2022(Version 1)available at Research Square (https://doi.org/10.21203/rs.3.rs-1430222/v1).
Funding
This study was supported by research grants from the Kameyama City Department of Community Medicine [No. J12061L005] and the Tsu City Department of Community Medicine [No. J12061L008].
Declaration of Interest
No conflict of interest, financial or otherwise, exists.
References
Aitken, S. A., Tinning, C. G., Gupta, S., Medlock, G., Wood, A. M., & Aitken, M. A. (2014). The importance of the orthopaedic doctors’ appearance: A cross-regional questionnaire-based study. The Surgeon, 12(1), 40-46. https://doi.org/10.1016/j.surge.2013. 07.002
Au-Yeung, P. K. K. (2005). SARS changed medical dress code. BMJ, 330(7505), 1450. https://doi.org/10.1136/bmj.330.7505.14 50-b
Banu, A., Anand, M., & Nagi, N. (2012). White coats as a vehicle for bacterial dissemination. Journal of Clinical and Diagnostic Research, 6(8), 1381-1384. https://doi.org/10.7860/JCDR/2012/42 86.2364
Baxter, J. A., Dale, O., Morritt, A., & Pollock, J. C. (2010). Bare below the elbows: Professionalism vs infection risk. The Royal College of Surgeons of England Bulletin, 92(7), 248-251. https://doi.org/10.1308/147363510X510581
Blumhagen, D. W. (1979). The doctor’s white coat. The image of the physician in modern America. Annals of Internal Medicine, 91(1), 111-116. https://doi.org/10.7326/0003-4819-91-1-111
Bond, L., Clamp, P. J., Gray, K., & Van Dam, V. (2010). Patients’ perception of doctors clothing: Should we really be ‘bare below the elbow’? The Journal of Laryngology and Otology, 124(9), 963-966. https://doi.org/10.1017/s0022215110001167
Brandt, L. J. (2003). On the value of old dress code in the new millennium. Archives of Internal Medicine, 163(11), 1277-1281. https://doi.org/10.1001/archinte.163.11.1277
Collins, A. M., Connaughton, J., & Ridgway, P. F. (2013). Bare below the elbows: A comparative study of a tertiary and district general hospital. Irish Medical Journal, 106(9), 272-275.
Edwards, R. D., Saladyga, A. T., Schriver, J. P., & Davis, K. G. (2012). Patient attitudes to surgeons’ attire in outpatient clinical setting: Substance over style. American Journal of Surgery, 204(5), 663-665. https://doi.org/10.1016/j.amjsurg.2009.09.001
Fischer, R. L., Hansen, C. E., Hunter, R. L., & Veloski, M. S. (2007). Does physician attire influence patient satisfaction in an outpatient obstetrics and gynecology setting? American Journal of Obstetrics and Gynecology, 196(2), e1-e5. https://doi.org/10.1016/ j.ajog.2006.09.043
Gherardi, G., Cameron, J., West, A., & Crossley, M. (2009). Are we dressed to impress? A descriptive survey assessing patient’s preference of doctors’ attire in the hospital setting. Clinal Medicine, 9(6), 519-524. https://doi.org/10.7861/clinmedicine.9-6-519
Gjerdingen, D. K., Simpson, D. E., & Titus, S. L. (1987). Patients’ and physicians’ attitudes regarding the physician’s professional appearance. Archives of Internal Medicine, 147(7), 1209-1212.
Gledhill, J. A., Warner, J. P., & King, M. (1997). Psychiatrists and their patients: Views on forms of dress and address. The British Journal of Psychiatry, 171, 228-232. https://doi.org/10.1192/bjp. 171.3.228
Gooden, B. R., Smith, M. J., Tattersall, S. J. N., & Stockler, M. R. (2001). Hospital patients’ views on doctors and white coat. The Medical Journal of Australia, 175(4), 219–222. https://doi.org/10.5694/j.1326-5377.2001.tb143103.x
Harnette, P. R. (2001). Should doctors wear white coat? The Medical Journal of Australia, 174(7), 343–344. https://doi.org/10.5694/j.1326-5377.2001.tb143310.x
Hennessy, N., Harrison, D. A., & Aitkenhead, A. R. (1993). The effect of the anaesthetist’s attire on patient attitudes. The influence of dress on patient perception of the anaesthetist’s prestige. Anesthesia, 48(3), 219-222. https://doi.org/10.1111/j.1365-2044 1 993.tb06905.x
Hippocrates. (1923). Hippocrates (W. H. S. Jones, Trans.) (Vol. 2). Harvard University Press.
Ikusaka, M., Kamegai, M., Sunaga, T., Narita, N., Kobayashi, H., Yonenami, K., & Watanabe, M. (1999). Patients’ attitude toward consultations by a physician without a white coat in Japan. Internal Medicine, 38(7), 533–536. https://doi.org/10.2169/internalmedici ne.38.533
Jacob, G. (2007). Uniform and workwear: An evidence base for developing local policy. National Health Service. https://data.parliament.uk/DepositedPapers/Files/DEP2009-0656/DEP2009-0656.pdf
Keenum, A. J., Wallace, L. S., & Stevens, A. R. (2003). Patients’ attitude regarding physical characteristics of family practice physicians. Southern Medical Journal, 96(12), 1190-1194. https://doi.org/10.1097/01.smj.0000077011.58103.c1
Keio University Hospital. (2014, May 20). Cool Biz no jisshi ni tsuite [About the implementation of Cool Biz]. Keio University Hospital. https://www.hosp.keio.ac.jp/oshirase/hosp/detail/38033/
King, C., & Infection Prevention and Control Nurse. (2022). Hand hygiene policy: Including bare below the elbows (Ver.9). Leicestershire Partnership National Health Service Trust. https://www.leicspart.nhs.uk/wp-content/uploads/2022/06/Hand-Hygiene-Policy-inc-bare-below-the-elbows.pdf
Kurihara, H., Maeno, T., & Maeno, T. (2014). Importance of physicians’ attire: factors influencing the impression it makes on patients, a cross-sectional study. Asia Pacific Family Medicine, 13(1), 2. https://doi.org/10.1186/1447-056x-13-2
Li, S. F., & Haber, M. (2005). Patient attitude toward emergency physician attire. The Journal of Emergency Medicine, 29(1), 1-3. https://doi.org/10.1016/j.jemermed.2004.12.014
Lightbody, K. A., & Wilkie, M. D. (2013). Perceptions of doctors’ dress code: ENT patients’ perspective. Clinical Otolaryngology, 38(2), 188-190. https://doi.org/10.1111/coa.12084
Menahem, S., & Shvaretzman, P. (1998). Is our appearance important to our patients? Family Practice, 15(5), 391-397. https://doi.org/10.1093/fampra/15.5.391
Ministry of the Environment. (2017, April 25). Heisei 29 nendo Cool Biz ni tsuite [About Cool Biz in 2017]. Ministry of the Environment, Japan. https://www.env.go.jp/press/103993.html
Nair, B. R., Mears, S. R., Hitchcock, K. I., & Attia, J. R. (2002). Evidence-based physicians’ dressing: A crossover trial. The medical Journal of Australia, 177(11-12), 681-682. https://doi.org/10.5694/j.1326-5377.2002.tb05017.x
Neinstein, L. S., Stewart, D., & Gordon, N. (1985). Effect of physician dress style on patient-physician relationship. Journal of Adolescent Health Car, 6(6), 456-459. https://doi.org/10.1016/S0 197-0070(85)80053-X
Nishihara, N., Haneda, M., & Tanabe, S. (2010). A study of office workers’ clothes and subjective evaluations in an office with a preset air-conditioning temperature of 28°C in summer. Journal of Home Economics of Japan, 61(3), 169-175. https://doi.org/10.114 28/jhej.61.169
Nishina, D., Murakawa, S., & Uemura, Y. (2007). A Study on the Effects of the Cool Biz introduced into the Regional Joint Government Buildings in Hiroshima. Technical papers of annual meeting, the Society of Heating, Air-Conditioning and Sanitary Engineers of Japan. 1463-1466. https://doi.org/10.18948/shasetai kai.2007.2.0_1463
Oyama, T., Tanaka, Y., & Haga, J. (1963). Color-affection and color-symbolism in Japanese and American students. The Japanese Journal of. Psychology, 34(3), 109-121. https://doi.org/ 10.4992/JJPSY.34.109
Palazzo, S., & Hocken, D. B. (2010). Patients’ perspectives on how doctors dress. The Journal of Hospital Infection, 74(1), 30-34. https://doi.org/10.1016/j.jhin.2009.08.021
Pronchik, D. J., Sexton, J. D., Melanson, S. W., Patterson, J. W., & Heller, M. B. (1998). Does wearing a necktie influence patient perceptions of emergency department care? The Journal of Emergency Medicine, 16(4), 541-543. https://doi.org/10.1016/s07 36-4679(98)00036-5
Rehman, S. U., Nietert, P. J., Cope, D. W., & Kilpatrick, A. O. (2005). What wear today? Effect of doctor’s attire on the trust and confidence of patient. The American Journal of Medicine, 118(11), 1279-1286. https://doi.org/10.1016/j.amjmed.2005.04.026
Shelton, C. L., Raistrick, C., Warburton, K., & Siddiqui, K. H. (2010). Can changes in clinical attire reduce likelihood of cross-infection without jeopardizing the doctor-patient relationship? The Journal of Hospital Infection, 74(1), 22-29. https://doi.org/10.10 16/j.jhin.2009.07.031
Takemura, Y., Atsumi, R., & Tsuda, T. (2008). Which medical interview behaviours are associated with patient satisfaction? Family Medicine, 40(4), 253-258. https://pubmed.ncbi.nlm.nih.gov/18382837/
Toquero, L., Aboumarzouk, O., Owers, C., Chiang, R., Thiagarajah, S., & Amin, S. (2011, April 02). Bare below the elbows-The patient’s perspective. Webmed Central. WebmedCentral. https://www.webmedcentral.com/article_view/1401
Wong, D., Nye, K., & Hollis, P. (1991). Microbial flora on doctors’ white coats. British Medical Journal, 303(6817), 1602-1604. https://doi.org/10.1136/bmj.303.6817.1602
Yamada, Y., Takahashi, O., Ohde, S., Deshpande, G. A., & Fukui, T. (2010). Patient’s preference for doctor’s attire in Japan. Internal Medicine, 49(15), 1521–1526. https://doi.org/10.2169/internalme dicine.49.3572
*Hideki Wakabayashi
Department of Community Medicine,
Mie University School of Medicine,
2-174, Edobashi,
Tsu, Mie,
514-8507, Japan
+81-59-231-5290
Email address: hidekiwaka@med.mie-u.ac.jp
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









