Practices, perceptions, attitudes, barriers and motivation and its impacts on research publication
Submitted: 9 February 2023
Accepted: 15 May 2023
Published online: 3 October, TAPS 2023, 8(4), 23-35
https://doi.org/10.29060/TAPS.2023-8-4/OA3006
Sethapong Lertsakulbunlue1, Kaophiphat Thammasoon2, Kanlaya Jongcherdchootrakul3, Boonsub Sakboonyarat3 & Anupong Kantiwong1
1Department of Pharmacology, Phramongkutklao College of Medicine, Thailand; 2Department of Personnel Administration Division, Phramongkutklao College of Medicine, Thailand; 3Department of Military and Community Medicine, Phramongkutklao College of Medicine, Thailand
Abstract
Introduction: Although medical research (MR) is constantly promoted, a global deficit of medical researchers has been noted. We aimed to explore the relationship among practice, perceptions, attitudes, barriers and motivation toward MR and its impacts on MR publication.
Methods: A cross-sectional study included 262 senior medical students and interns. An electronic, standardised Likert scale questionnaire was used to collect the data. Binary logistic regression was used to determine the odds ratio between characteristics and MR publication. Confirmatory factor analysis was used to confirm the loading factor of each question, and structural equation modeling (SEM) was used to investigate the relationship between latent variables and MR publication.
Results: Cronbach’s alpha revealed a good internal reliability of 0.93. The accumulated grade point average did not differ between those who had published and those who had not. MR presentations were strongly associated with MR publication. SEM showed that attitudes (0.71, p<0.001) and perceptions (0.27, p<0.001) had a direct effect on practices. Practices (0.49, p<0.001) and attitudes (0.30, p<0.001) had a direct effect on motivation, while motivation had a total effect = 0.36, p<0.001 on MR publication through MR presentation as a mediator.
Conclusion: Positive attitudes and perceptions might lead to positivity in the intention to practice MR, which would lead to motivation and finally increase the odds of MR publication. Different approaches to promote excitement and perceptions in MR learning should be encouraged by teachers and faculty members.
Keywords: Medical Research, Students, Perceptions, Attitudes, Barriers, Motivation
Practice Highlights
- Enjoyment and excitement should be promoted while learning medical research.
- Medical research experiences enhanced publication, particularly medical research presentations.
- Extracurricular medical research activities should be routinely promoted.
- Facilitators in medical research might be tailor-made for each individual.
- Regular meetings regarding medical research with mentors or role models should be held.
I. INTRODUCTION
Health-related research is constantly promoted and has gained great importance over time (Sobczuk et al., 2022). However, a global shortage of medical researchers was noted despite an increasing demand for them (Funston et al., 2016). For example, in the US, the proportion of medical researchers has declined from approximately 4.7% to 1.5% in the 1980s and 2014, respectively (Carberry et al., 2021; Davila, 2016; Puljak, 2007). Several barriers toward conducting medical research (MR) have been reported among undergrads and postgraduates. For instance, lack of allotted time, lack of physician engagement in research early during medical students’ training, and lack of mentoring and guidance (Bonilla-Escobar et al., 2017; El Achi et al., 2020; Habineza et al., 2019; Okoduwa et al., 2018). To resolve these problems, medical education has globally incorporated research methods and epidemiology into its curriculum (Carberry et al., 2021). Nevertheless, only a minority of medical students had reached the primary goal of research, namely publishing (Bonilla-Escobar et al., 2017; Carberry et al., 2021; Laidlaw et al., 2012).
Factors associated with MR publication have been identified. Students from highly ranked undergraduate institutions were more likely to achieve publication. Mentors also played an important role in increasing the likelihood of publication. For example, a student working with a mentor with a PhD degree or a mentor with prior publication(s) with prior mentee(s) increases the chance of achieving publication (Parker et al., 2021). Medical students participating in an extracurricular scientific activity, such as the Scientific Society of Medical Students, or who take a scientific writing skills course, were also associated with greater odds of producing a scientific publication (Valladares-Garrido et al., 2022).
One of the main reasons researchers conduct a study is because of what they believe (Lev et al., 2010). Attitudes toward and barriers against health research influence research success (Lev et al., 2010; Memarpour et al., 2015; Osman, 2016). Attitudes and motivations toward a particular type of study also showed a positive relationship with achievement (Ma & Xu, 2004; Özer, 2020; Simpson & Oliver, 1990). Furthermore, a theory of success describes perception leading to passion, and the continuation of passion leading to obsession, which drives an individual to succeed (Dange, 2016; Schellenberg et al., 2022).
Previously, several studies reported descriptive data on attitudes, practices, knowledge levels, perceptions, motivation and barriers involving research among medical and science students (AlGhamdi et al., 2014; Al-Shalawy & Haleem, 2015; Arif et al., 2018; El Achi et al., 2020; Habineza et al., 2019; Memarpour et al., 2015; Osman, 2016; Pallamparthy & Basavareddy, 2019). Even though these factors are known to affect one’s behaviour, to our knowledge, research on whether these factors are associated with research publications among medical students is scarce.
Without research, no breakthroughs can be achieved in managing disease. Therefore, strategies to enhance medical students’ appreciation of research and publication should be promoted. As a step toward this goal, our study aimed to determine the relations between MR practices, perceptions, attitudes, barriers and motivation toward medical research and their effect on MR publications among senior medical students and internists graduated from Phramongkutklao College of Medicine, Thailand. Furthermore, we also explore the differences in the characteristics and MR experiences of the participants between the publishing group and the non-publishing group. The goal involved influencing future research and actions to increase research publications among physicians in the country and contribute to medical practices.
II. METHODS
A. Study Design and Subjects
A cross-sectional study based on a self-administered survey was conducted at Phramongkutklao College of Medicine (PCM), Bangkok, Thailand. The survey was distributed among senior medical students, including fourth-, fifth-, and sixth-year students and internists who graduated from PCM. The total number of senior medical students and internists was 292 and approximately 250 interns, respectively. The curriculum at PCM is spread out over six years, with the first three being pre-clinical years spent studying basic science and the last three being clinical years spent developing clinical experiences. An introductory module about MR is mandatory in three years of the curriculum in the third, fourth, and sixth years of medical school. Firstly, third-year medical students learn the basics of MR, such as basic study designs focusing on quantitative methods, data analysis, and research proposal development. Furthermore, students learn about public health aspects, including community participation. Secondly, fourth-year medical students learn more about advanced study designs and are more focused on conducting a study and multivariate analysis. Fourth-year students were divided into eight groups of approximately twelve to conduct a community-based research proposal before finalizing their project as a report. Finally, sixth-year medical students were divided into pairs or a group of three to conduct medical research to improve medical care in a community hospital setting. Then the research is presented, and a manuscript report is submitted. However, an MR publication was not mandatory. After they graduated, the students were sent to both Thai Army hospitals and government hospitals run by the Ministry of Public Health to work as interns.
The present study included senior medical students and internists due to their similar MR experiences. First, both groups were enrolled within the same curriculum paradigm. Second, the MR presentation and publications are according to the willingness of the student, as MR publications and presentations are not mundane. Finally, almost all the published research among the population is from projects developed during their fourth and sixth years as medical students. Therefore, several projects were published during the internship.
B. Data Collection
We used an electronic standardised questionnaire, including six parts: short answer questions for obtaining demographic data; a 5-score Likert scale questionnaire on practice, perceptions, attitudes, barriers, and motivation toward MR. The questionnaire was translated using related published work that is relevant to this paper, as well as the investigators’ experience and context of PCM (El Achi et al., 2020; Funston et al., 2016; Habineza et al., 2019; Ichsan et al., 2018; Kamwendo, 2002; Okoduwa et al., 2018; Pallamparthy & Basavareddy, 2019). In addition, five expert professors examinedthe content validity and reliability of the questionnaire; pilot testing was conducted among 66 first year medical students and Cronbach’s alpha score ranged from 0.74-0.93.Then the questionnaire was launched in November and December of 2022 as a Google Form and advertised via social media to the study population. Information sheets, objectives, and methods of the study were provided on the first page of the Google Form, which participants were asked to read carefully before agreeing to participate. The questionnaire was then self-completed and took, on average, about 10–15 minutes to complete. The finalised Cronbach’s alphas were 0.83, 0.84, 0.74, 0.89, 0.88, and 0.93 for practices, perceptions, attitudes, barriers, motivation and overall questions, respectively.
Practice was defined as their willingness or intention to practice MR (El Achi et al., 2020). Perceptions are how the student perceives the importance of MR, while attitude is how they feel about conducting MR (El Achi et al., 2020; Funston et al., 2016). Barriers are defined as what the students perceive as being resistant to conducting MR; on the other hand, motivations are what they perceive as facilitating conducting MR (Habineza et al., 2019; Okoduwa et al., 2018).
C. Statistical Analysis
All data were downloaded from Google Forms, and data analyses were performed using StataCorp, 2021, Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC. A frequency distribution of demographic characteristics was performed to describe the study subjects. Categorical data were presented as percentages, and continuous variables were presented as means and standard deviations (SD). Univariable and multivariable logistic regression analysis was used to determine the odds ratio (OR) and adjusted odds ratio (AOR) with a 95% confidence interval (CI) of the association between the characteristics and MR experiences of the participants and the MR publication. All statistical tests were two-sided, and a p-value less than 0.05 was considered statistically significant.
The structural equation modeling (SEM) using maximum likelihood extraction was done to find out how the latent variables, including practice, perceptions, attitudes, barriers, and motivation, were related and what effect it had on MR publications. The procedure is comprised of two steps. The first is validating the measurement model, which is carried out primarily using confirmatory factor analysis (CFA), and the other is fitting the structural model, which is achieved primarily through path analysis of latent variables. CFA was applied to demonstrate the impact of each question (observed variable) on different beliefs toward MR (latent variable) and presented as a lambda. Questions with a low factor loading (below 0.60) were excluded from the SEM. During the SEM construction, questions with factor loadings below 0.60 were also removed. In the final model, there are 17 observed variables included within the SEM. The samples/observed variable were 15.41, which is more than 10, indicating adequate sample size for SEM (Wolf et al., 2013). The SEM was carried out to investigate the relationship among latent variables and their impact on MR publication in our study population.The six following indices were used to evaluate model fit: (1) the chi-square test, χ2; (2) the chi-square test over degree of freedom (df), χ2/df (3) the comparative fit index, CFI; (4) the Tucker–Lewis index, TLI (5) the root-mean square error of approximation, RMSEA; and (6) the root-mean square residual, (SRMR). All these indices indicated a proposed fit for SEM data. A χ2/df lower than 2, CFI greater than 0.95, TLI greater than 0.95, RMSEA less than 0.06 and SRMR less than 0.06 each indicated a good fit between the data and the hypothesised model.
III. RESULTS
A. Characteristic of Participants
Table 1 demonstrates the characteristics of participants stratified by MR publishing. A total of 139 senior medical students and 123 interns participated in the survey. The response rate was 47.6% and 49.2% for senior medical students and interns, respectively. Over one-fifth (22.1%) of the participants had published MR and were mostly internists (81.0%). Approximately 60% of the participants were male, corresponding to an enrolment at PCM of 60 male and 40 female students. The accumulated grade point average (GPAX) was approximately the same at 3.4±0.3 among both published and those who had not published. Regarding, MR experience or roles served during medical student years, being a group leader (AOR: 2.12, 95% CI: 0.97 to 4.64, p=0.06) was associated with MR publishing. Finally, those having experience in MR presentation, whether oral or poster, and international or national presentation, were strongly associated with MR publishing, with adjusted odds ratios of 4.34 (p<0.001) shown in Table 2.
|
Characteristics |
Non-Published |
Published |
|
n (% of 204) |
n (% of 58) |
|
|
Demographics |
||
|
Sex |
||
|
Male |
119 (58.3) |
37 (63.8) |
|
Female |
85 (41.7) |
21 (36.2) |
|
Educational level |
||
|
Clinical year |
128 (62.7) |
11 (19.0) |
|
Intern |
76 (37.3) |
47 (81.0) |
|
Accumulated grade point average (GPAX) |
||
|
Mean ± SD |
3.4±0.3 |
3.4±0.3 |
|
Medical research participation |
||
|
MR elective |
59 (28.9) |
15 (25.9) |
|
Time spent on MR (hours/week) |
||
|
<1 |
119 (58.3) |
27 (46.6) |
|
1-5 |
56 (27.5) |
17 (29.3) |
|
5-10 |
15 (7.4) |
7 (12.1) |
|
>10 |
14 (6.9) |
7 (12.0) |
|
Extra curriculum research activity |
39 (19.1) |
23 (39.7) |
|
Academic club activity |
30 (14.7) |
13 (22.4) |
|
MR experience during medical student |
||
|
Group leader |
45 (22.1) |
24 (41.4) |
|
Design MR |
89 (43.6) |
34 (58.6) |
|
Proposal writing |
142 (69.6) |
45 (77.6) |
|
Data enter |
126 (51.5) |
41 (70.7) |
|
Data analysis |
99 (48.5) |
34 (58.6) |
|
Literature review |
125 (61.3) |
42 (72.4) |
|
Manuscript writing |
76 (37.3) |
33 (56.9) |
|
None |
7 (3.4) |
2 (3.4) |
|
National MR presentation |
||
|
Oral presentation |
23 (11.3) |
22 (37.9) |
|
Poster presentation |
22 (10.8) |
22 (37.9) |
|
International MR presentation |
||
|
Oral presentation |
7 (3.4) |
8 (13.8) |
|
Poster presentation |
9 (4.4) |
15 (25.9) |
|
Published national MR |
0 (0) |
29 (50.0) |
|
Published international MR |
0 (0) |
37 (63.8) |
MR: Medical Research
Table 1. Characteristics of participants stratified by medical research publishing experience (N=262)
|
Characteristics |
Non-Published |
Published |
OR |
95% CI |
p-value |
AOR |
95% CI |
p-value |
|
n (% of 204) |
n (% of 58) |
|||||||
|
Sex |
||||||||
|
Male |
119 (58.3) |
37 (63.8) |
ref |
ref |
||||
|
Female |
85 (41.7) |
21 (36.2) |
0.79 |
0.43-1.45 |
0.455 |
0.76 |
0.37-1.56 |
0.458 |
|
Educational level |
||||||||
|
Clinical year |
128 (62.7) |
11 (19.0) |
ref |
ref |
||||
|
Intern |
76 (37.3) |
47 (81.0) |
3.09 |
1.74-5.50 |
<0.001 |
6.67 |
3.12-14.28 |
<0.001 |
|
Accumulated grade point average (GPAX) |
||||||||
|
Mean±SD |
3.4±0.3 |
3.4±0.3 |
1.02 |
0.40-2.59 |
0.971 |
0.417 |
0.12-1.41 |
0.159 |
|
Extra curriculum research activity |
39 (19.1) |
23 (39.7) |
2.78 |
1.48-5.23 |
0.002 |
1.47 |
0.62-3.46 |
0.379 |
|
MR experience during medical student |
||||||||
|
Group Leader |
45 (22.1) |
24 (41.4) |
2.49 |
1.34-4.63 |
0.004 |
2.12 |
0.97-4.64 |
0.060 |
|
MR presentation |
||||||||
|
No |
170 (83.3) |
27 (46.6) |
ref |
ref |
||||
|
Yes |
34 (16.7) |
31 (53.5) |
5.74 |
3.05-10.82 |
<0.001 |
4.34 |
1.99-9.47 |
<0.001 |
MR: Medical Research, OR: Odds Ratio, AOR: Adjusted Odds Ratio, CI: Confidence interval
Table 2. Univariable and multivariable analysis of characteristics and medical research experiences by medical research publishing experience (N=262)
B. Confirmatory Factor Analysis of Practices, Perceptions, Attitudes, Barriers and Motivation toward Medical Research
Table 3 demonstrates the confirmatory factor analysis (CFA) of practices, perceptions, attitudes, barriers and motivation Likert scores and MR publishing experience. In the practice section, all questions had a loading factor of approximately 0.80. The loading factors for perception range from 0.74 to 0.79, except for two questions: (1) research or publication should be mandatory and (2) research experience should be a criterion for residency training. For the attitude section, the CFA found that MR is exciting and MR is enjoyable, with high impacts of 0.89 and 0.87, respectively, followed by MR being valuable and essential for the medical profession, with loading factors of 0.58 and 0.54, respectively. However, for the questions where MR is complicated and time-consuming, the loading factor was relatively low, under 0.30. Regarding barriers, lack of exposure and opportunities, training and support, mentoring and guidance, and lack of personal knowledge of the research process all had a high loading factor of over 0.70. Lack of statistical support, funding, and lack of rewards or motivations had relatively lower loading factors between 0.60 and 0.69. For motivation, pursuit of further education, pursuit of personal interest, improving their potential in research skills, having mentor guidance/role model and to be a part of solving medical problems in society had high loading factors over 0.70.
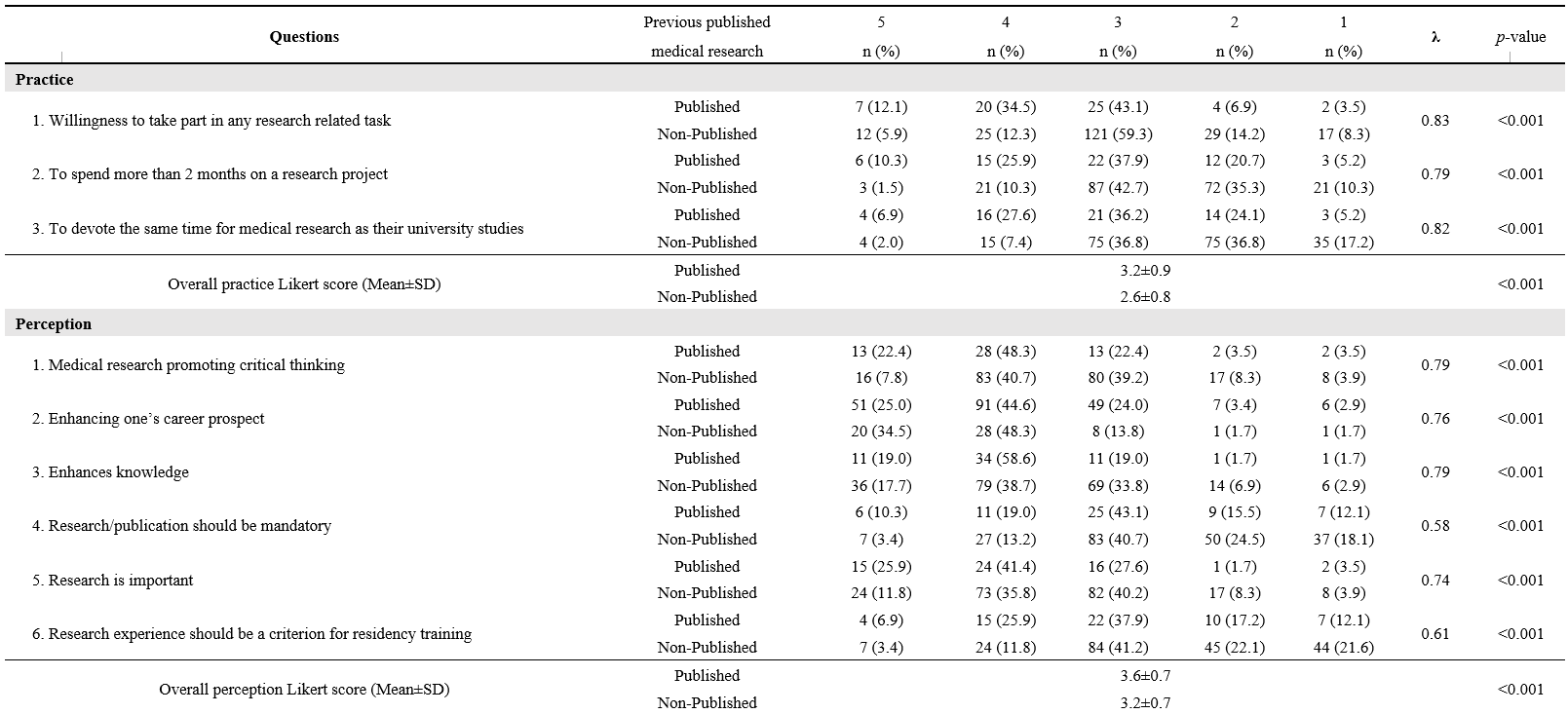
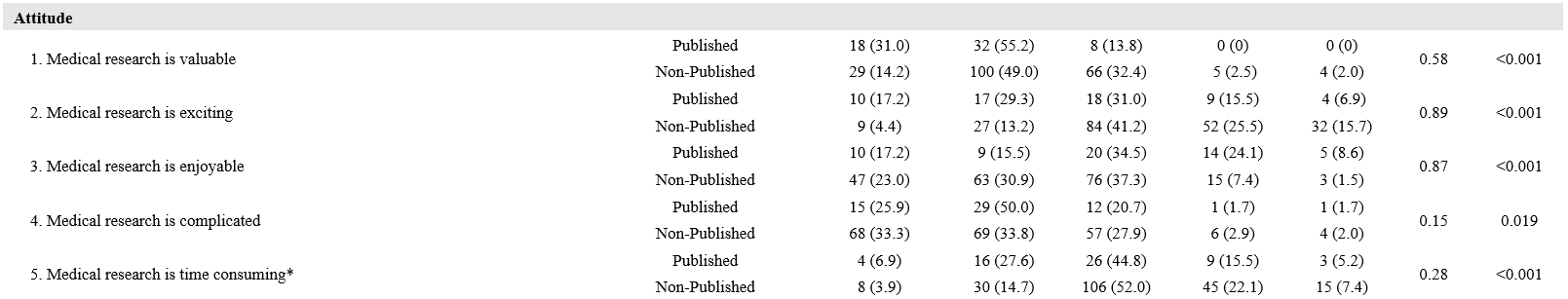
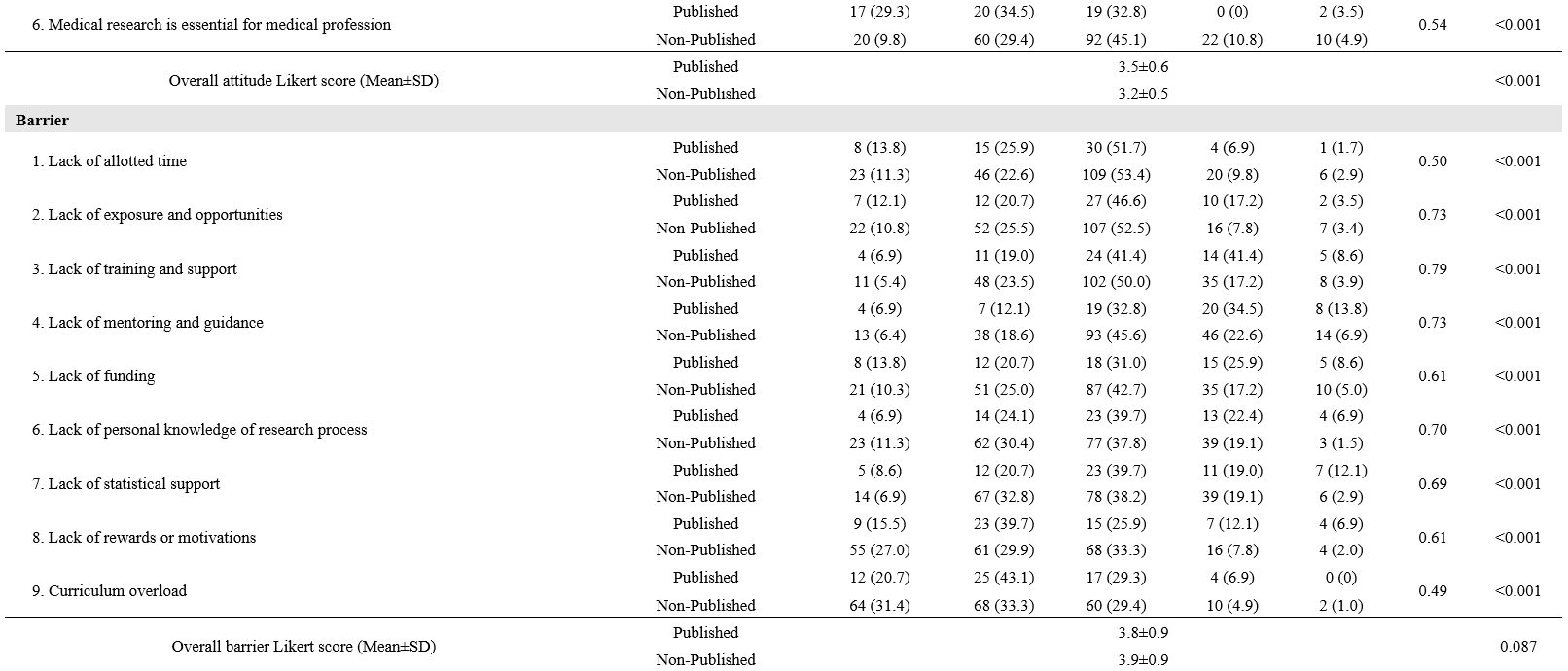
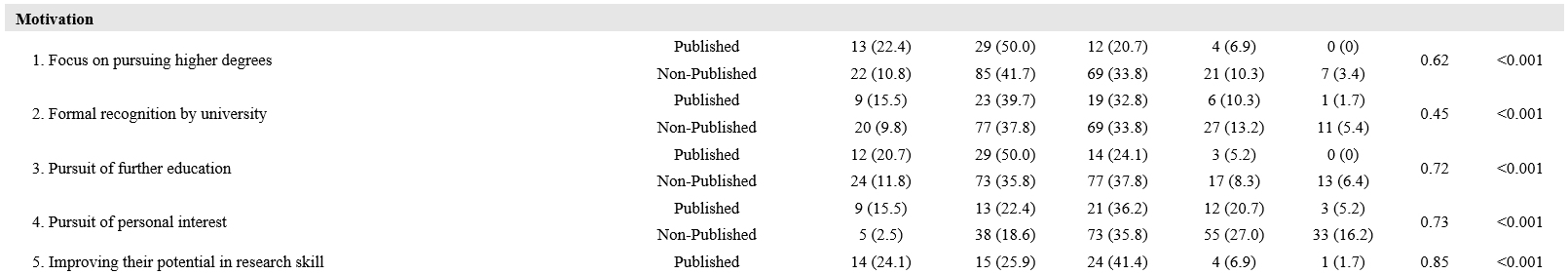
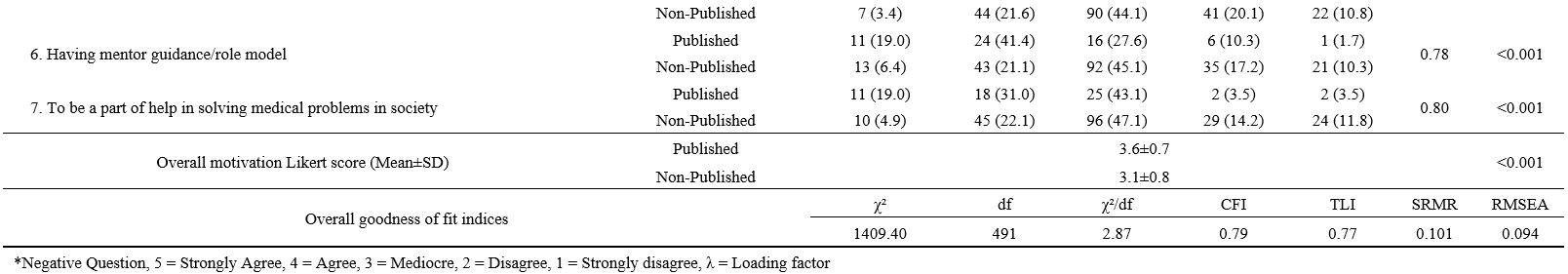
Table 3. Confirmatory factor analysis of practice, perception, attitude, barrier and motivation Likert-score and medical research publishing experience
C. SEM of Practices, Perceptions, Attitudes, Barriers and Motivation and MR Publishing
The SEM is developed from five latent variables, leading to the outcome, including medical research presentation and publication (Figure 1). We found that perception has a direct effect on both practices (0.27, p<0.001) and motivation (0.12, p= 0.087). Perceptions and attitudes also correlated (0.57, p<0.001). Practices and attitudes have a direct effect on motivation, 0.49 and 0.30, respectively (p<0.001 for both). The indirect effect of attitudes through practices on motivation was 0.71 * 0.49 = 0.35, all coefficients p<0.001. Practices also exhibited a direct negative effect on barriers (-0.13, p= 0.072). Regarding our primary outcome, both motivation and, surprisingly, barriers also revealed a positive direct effect on MR publishing (0.28, p<0.001 for motivation and 0.15, p= 0.014 for barriers). The MR presentation experience also showed a direct effect on MR publication (0.26, p<0.001). Furthermore, MR presentation also acted as a mediator for motivation, with an indirect effect of 0.08 and a total effect of motivation on MR publication of 0.36. The SEM model provided a good fit for the data (χ²/df= 1.67, CFI= 0.96, TLI= 0.95, RMSEA= 0.05, SRMR= 0.05).
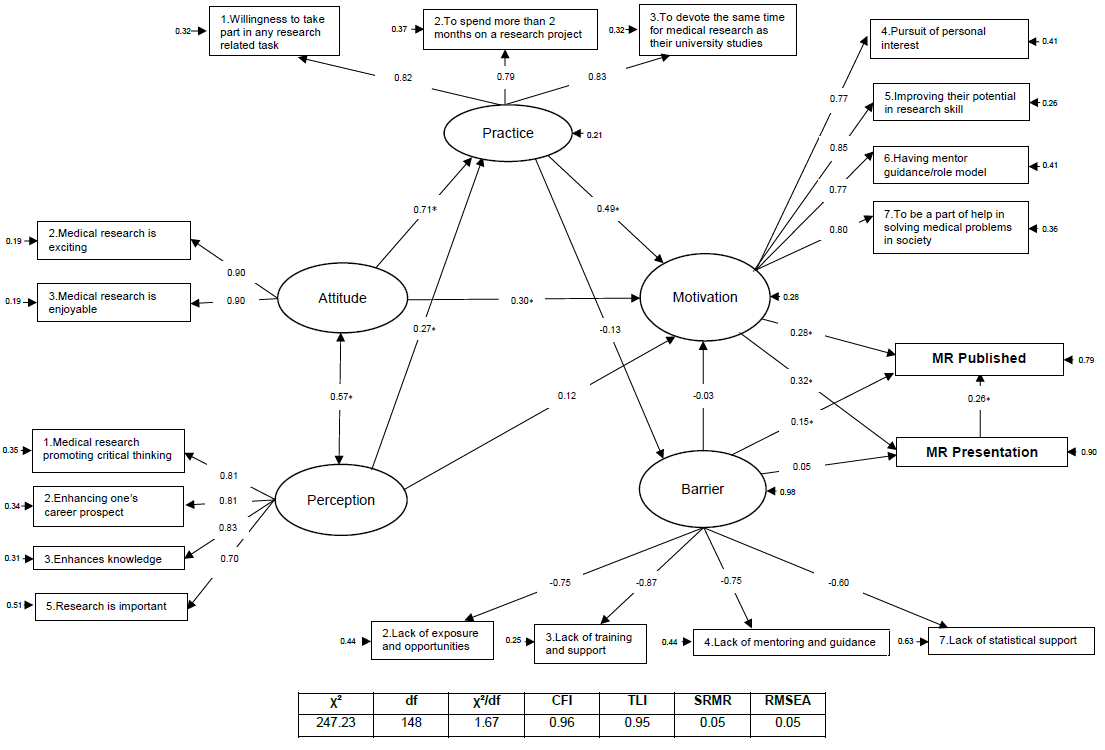
*= P<0.05
Figure 1. SEM of practices, perceptions, attitudes, barriers and motivation and MR publishing
IV. DISCUSSION
We successfully enrolled 139 PCM senior medical students, and 123 interns graduated from PCM. This study is the first to formulate a SEM on the relationship between practices, perceptions, attitudes, motivation and barriers to MR publication and presentation. We found that attitudes, practices and motivation significantly contribute to MR publication and presentation. The roles and experiences that medical students have in medical research during their medical student years are also important to the success of MR publications. However, because our population only includes those who have studied or are studying at PCM, additional external validation may be required.
This study described how baseline characteristics and MR experiences were associated with MR publication. Unsurprisingly, a higher proportion of interns had published MR. GPAX, on the other hand, were not associated with MR publication, which is a common factor in a relative study with positive associations toward perceptions, attitudes and practices (El Achi et al., 2020). A large study in China also reported that research engagement was associated with improving overall learning outcomes (Zhang et al., 2022). This controversy may be explained by two reasons. First, the time required for developing MR and publications is large and might interfere with normal curriculum activity. A study in Colombia noted that their students believed that they could obtain higher GPAs if they were not involved in research (Bonilla-Escobar et al., 2017). The latter is that MR skills and academic skills might not completely overlap. While MR engagement might improve science, scholarship, and professionalism, other domains, such as clinical practice, require more time and effort to learn (Zhang et al., 2022).
MR experiences and roles during MR learning also play an important part in MR publication. Experience in MR presentation was strongly associated with MR publication. This may be partially explained by the student’s readiness before the research presentation; students need to be highly knowledgeable about their own research, and knowledge is a key to success and behavioural change (Bettinghaus, 1986; Pengpid et al., 2016). Furthermore, presentation requires planning, preparation, creating visual aids, and practicing one’s presentation skills. The effort and time spent on this process might be motivation to achieve a higher goal, namely publication. Our study demonstrates that MR presentations, whether nationally, internationally, oral, or poster, are highly associated with MR publication. Thus, MR presentations should be promoted.
Those who had been group leaders had a higher chance of MR publication. During the PCM curriculum, the group leader for MR conduct was never assigned and was elected in each group. Northouse mentioned two forms of leadership: assigned and emergent. Those assigned leadership positions were given the role of group leader. When an individual is perceived as one of the most influential members of a group or organization, that person is exhibiting emergent leadership (Northouse, 2021). Medical leadership development was seen to improve outcomes at the individual, organizational and clinical levels (Lyons et al., 2021). Several leadership training programs in medicine and clinical practices were widely visible. However, to our knowledge, no curriculum focusing on medical research leadership was available.
Perception is described as a method for identifying and interpreting the environment and the meaning of sensual motivations. Cognition may influence perception, which can also occur subconsciously and without cognizance (Saini et al., 2020). Some literature has been carried out showing perceptions, attitudes, and motivation toward research among medical students, in which those with positive perceptions mostly had positive attitudes and motivation (AlGhamdi et al., 2014; El Achi et al., 2020; Osman, 2016). These were similar to our research showing that perception impacts positively on practices and motivation.
In line with the current study, the theory of planned behaviour describes that one’s attitude and how they perceive the behaviour directly affect their intention to perform the behaviour (Bosnjak et al., 2020). The SEM also demonstrated that perception and attitude directly affect the population’s intention to conduct MR (practice). Moreover, a study in Turkey on the predictiveness of attitude and motivation on achievement (vocational English course scores) found a significant positive relationship between attitude and motivation, attitude and achievement, and motivation and achievement (Özer, 2020). Therefore, a positive attitude may positively impact their motivation and their willingness to practice MR. The feeling that MR is exciting and enjoyable had the greatest impact on the attitude domain. Hence, activities that increase the excitement and joy of conducting MR should be encouraged.
The main factors impacting MR publication are motivation, practices, attitudes and perceived barriers. Based on the health-belief model (HBM), providing motivation as needed might help students overcome the triggers of MR barriers so that correct thoughts and perceptions about MR will arise. Thus, techniques derived from motivational interviews might be a useful option for encouraging students toward MR publication (Tober, 2013). One of the most important motivations in our study is having a mentor or role model, and the lack of a mentor constitutes a high-impact barrier. Therefore, mentors should play an important role in guiding their students toward research success. Based on motivational interview techniques, active listening might be the key skill for mentors to better understand their students’ motivations and empower them toward success (Rollnick et al., 2010).
Surprisingly, our study showed that perceived barriers had a positive impact on MR publication. The perception of a barrier greatly influences the likelihood of an individual’s uptake of that behaviour (Becker & Maiman, 1975). Usually, a barrier is a resistance to achieving a goal, which negatively affects achievement. However, the barriers included in our study consisted of a lack of exposure and opportunities, training and support, mentoring and guidance, and statistical support. As a result, those who had not yet published any medical research may not have had the prestige of encountering these barriers, which is why they are perceived as insignificant.
The practice domain included three questions: (1) willingness to participate in any research-related task; (2) willingness to spend more than two months on a research project; and (3) willingness to devote the same amount of time to medical research as they did to their university studies, indicating a willingness to practice medical research. Willingness is the quality or state of being prepared to accomplish something. A study in China about speaking English demonstrated that the willingness to communicate is directly related to motivation and mastery approach (Turner et al., 2021). Furthermore, passion and obsession are what drive an individual to succeed (Dange, 2016).
In view of all the factors presented, mentors have an important role to play in guiding and facilitating the students’ acquisition of adequate experience in medical research during their medical school years. A good extracurricular MR learning environment might be needed to ensure statistical confidence and exposure to conducting research. Actively listening to students and empowering and motivating them to break through barriers may result in successful MR publications. In addition, a different approach to learning MR might be needed to promote attitudes, perceptions and motivations toward MR. According to Self-Determination Theory (SDT), when students perceive that the primary purpose of learning is to obtain external rewards, such as exam grades, they may perform less well due to a detrimental effect on their intrinsic motivation (Deci et al., 1999).
SDT revealed that three basic needs must be fulfilled to empower one’s attitude and motivation, including autonomy, competence, and a feeling of belonging (Deci et al., 1999). To promote these basic needs, faculty members could provide extracurricular research time, give choice to research topics and mentors, and hire students to be research assistants, if possible, to promote their autonomy (Rosenkranz et al., 2015). Competence could be enhanced by early research skills introduction and practical training (Rosenkranz et al., 2015). Research mentors may play a crucial role in fostering a sense of belonging toward MR by promoting well-functioning group work through guidance and evaluation (Dorrance et al., 2008). Furthermore, portfolios, logbooks and reflective journals are particularly useful to improve the students’ attitude and motivation (Taylor & Hamdy, 2013). Constant positive feedback from mentors during MR activities is encouraged to improve the learning environment (Peifer et al., 2020). A different approach to learning MR might also benefits the MR learning environment, for example, through game-based learning and other collaborative learning models (Blakely et al., 2009).
The present study encountered several limitations. First, the study included only senior medical students and interns who graduated from PCM, so the model might not be accurately applied to other universities with different curricula and further validation might be needed. Even though most participants who had published a MR were interns (81%), the medical research published was composed while they were medical students. Second, the study was a cross-sectional study, and causal relationships were unavailable. However, according to PCM curricula, for most participants, the MR presentation and their experience with medical research came before the MR publication. Furthermore, personal beliefs change over time, and recall bias might have affected the study results. (Seitz et al., 2017). The beliefs elicited by the questionnaire comprised the participants’ current beliefs, rather than beliefs formed during their participation in medical research publications. As a result, our study investigated only the participants’ current beliefs and their impact on the publication of medical research. A further prospective cohort or qualitative study on whether the students’ current beliefs toward MR are related to successful MR publication is encouraged. Finally, because only participants who volunteered to take part in the study were included, selection bias may also be a significant limitation of this study. Our study had considerable strengths, there had been no reports describing practices, perceptions, attitudes, motivation and barriers toward medical research. However, this is the first study to formulate a SEM model displaying factors related to MR publication.
V. CONCLUSION
Medical research experience and positive practices or willingness, perception, attitude, and motivation in medical research might pave the road to a successful MR publication. Medical research experience and extracurricular activities should be supported by both teachers and faculties through active policies. A different approach to medical research learning might also be needed to promote enjoyment and excitement. Finally, external validation needs to be explored to generalise the model.
Notes on Contributors
SL reviewed the literature, designed the study, collected the data, data analysis and wrote the manuscript. KT, KJ and BS collected the data, developed the methodology framework and developed the manuscript. AK reviewed the literature, designed the study, data analysis and wrote the first draft.
Ethical Approval
The study was approved by the Medical Department Ethics Review Committee for Research in Human Subjects, Institutional Review Board, Royal Thai Army (Approval no. S060q/65_Exp), according to the international guidelines including the Declaration of Helsinki, the Belmont Report, CIOMS Guidelines, and the International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use – Good Clinical Practice (ICH-GCP). A documentation of informed consent was used, and was granted permission by the Institutional Review Board, RTA Medical Department.
Data Availability
The datasets used and/or analysed during the current are available from https://doi.org/10.6084/m9.figshare.22128725
Acknowledgement
We thank professors Mathirut Mungthin, Ram Rangsin Panadda Hattachote, Phunlerd Piyaraj and Picha Suwannahitatorn for validating our questionnaire and providing support. This work would not have been possible without the active support of Phramongkutklao College of Medicine and its academic leaders.
Funding
The authors report that there is no funding associated with the work featured in this article.
Declaration of Interest
The authors declare they have no competing interests.
References
AlGhamdi, K. M., Moussa, N. A., AlEssa, D. S., AlOthimeen, N., & Al–Saud, A. S. (2014). Perceptions, attitudes and practices toward research among senior medical students. Saudi Pharma- ceutical Journal, 22(2), 113–117. https://doi.org/10.1016/j.jsps.2013.02.006
Al–Shalawy, F. A.-N., & Haleem, A. (2015). Knowledge, attitudes and perceived barriers towards scientific research among undergraduate health sciences students in the central province of Saudi Arabia. Education in Medicine Journal, 7(1), e16-e21. https://doi.org/10.5959/eimj.v7i1.266
Arif, A., Siddiqui, M. A., Aziz, K., Shahid, G., Shiekh, A., & Fahim, M.F. (2018). Perception towards research among undergraduate physical therapy students. Biometrics & Biostatistics International Journal, 7(3), 171–175. https://doi.org/10.15406/bbij.2018.07.00206
Becker, M. H., & Maiman, L. A. (1975). Sociobehavioral determinants of compliance with health and medical care recommendations. Medical Care, 13(1), 10–24. https://doi.org/10.1097/00005650–197501000–00002
Bettinghaus, E. P. (1986). Health promotion and the knowledge–attitude–behavior continuum. Preventive Medicine, 15(5), 475–491. https://doi.org/10.1016/0091–7435(86)90025–3
Blakely, G., Skirton, H., Cooper, S., Allum, P., & Nelmes, P. (2009). Educational gaming in the health sciences: Systematic review. Journal of Advanced Nursing, 65(2), 259–269. https://doi.org/10.1111/j.1365-2648.2008.04843.x
Bonilla–Escobar, F. J., Bonilla–Velez, J., Tobón–García, D., & Ángel–Isaza, A. M. (2017). Medical student researchers in Colombia and associated factors with publication: A cross–sectional study. BMC Medical Education, 17(1), Article 254. https://doi.org/10.1186/s12909–017–1087–9
Bosnjak, M., Ajzen, I., & Schmidt, P. (2020). The theory of planned behavior: Selected recent advances and applications. Europe’s Journal of Psychology, 16(3), 352–356. https://doi.org/10.5964/ejop.v16i3.3107
Carberry, C., McCombe, G., Tobin, H., Stokes, D., Last, J., Bury, G., & Cullen, W. (2021). Curriculum initiatives to enhance research skills acquisition by medical students: A scoping review. BMC Medical Education, 21(1), Article 312. https://doi.org/10.1186/s12909–021–02754–0
Dange, J. K. (2016). Perception, passion and obsession: The three elements of theory of success. International Journal of Advanced Education and Research, 1(7), 1–3.
Davila, J. R. (2016). The physician–scientist: Past trends and future directions. Michigan Journal of Medicine, 1(1), 66-73. https://doi.org/10.3998/mjm.13761231.0001.112
Deci, E. L., Koestner, R., & Ryan, R. M. (1999). A meta-analytic review of experiments examining the effects of extrinsic rewards on intrinsic motivation. Psychological Bulletin, 125(6), 627–668. https://doi.org/10.1037/0033-2909.125.6.627
Dorrance, K. A., Denton, G. D., Proemba, J., La Rochelle, J., Nasir, J., Argyros, G., & Durning, S. J. (2008). An internal medicine interest group research program can improve scholarly productivity of medical students and foster mentoring relationships with internists. Teaching and Learning in Medicine,20(2), 163–167. https://doi.org/10.1080/10401330801991857
El Achi, D., Al Hakim, L., Makki, M., Mokaddem, M., Khalil, P. A., Kaafarani, B. R., & Tamim, H. (2020). Perception, attitude, practice and barriers towards medical research among undergraduate students. BMC Medical Education, 20(1), Article 195. https://doi.org/10.1186/s12909–020–02104–6
Funston, G., Piper, R. J., Connell, C., Foden, P., Young, A. M. H., & O’Neill, P. (2016). Medical student perceptions of research and research–orientated careers: An international questionnaire study. Medical Teacher, 38(10), 1041–1048. https://doi.org/10.3109/0142159X.2016.1150981
Habineza, H., Nsanzabaganwa, C., Nyirimanzi, N., Umuhoza, C., Cartledge, K., Conard, C., & Cartledge, P. (2019). Perceived attitudes of the importance and barriers to research amongst Rwandan interns and pediatric residents – A cross–sectional study. BMC Medical Education, 19(1), Article 4. https://doi.org/10.1186/s12909–018–1425–6
Ichsan, I., Wahyuniati, N., McKee, R., Lobo, L., Lancaster, K., & Redwood–Campbell, L. (2018). Attitudes, barriers, and enablers towards conducting primary care research in Banda Aceh, Indonesia: A qualitative research study. Asia Pacific Family Medicine, 17(1), Article 8. https://doi.org/10.1186/s12930–018–0045–y
Kamwendo, K. (2002). What do Swedish physiotherapists feel about research? A survey of perceptions, attitudes, intentions and engagement. Physiotherapy Research International, 7(1), 23–34. https://doi.org/10.1002/pri.238
Laidlaw, A., Aiton, J., Struthers, J., & Guild, S. (2012). Developing research skills in medical students: AMEE Guide No. 69. Medical Teacher, 34(9), 754–771. https://doi.org/10.3109/0142159X.2012.704438
Lev, E. L., Kolassa, J., & Bakken, L. L. (2010). Faculty mentors’ and students’ perceptions of students’ research self-efficacy. Nurse Education Today, 30(2), 169–174. https://doi.org/10.1016/j.nedt.2009.07.007
Lyons, O., George, R., Galante, J. R., Mafi, A., Fordwoh, T., Frich, J., & Geerts, J. M. (2021). Evidence–based medical leadership development: A systematic review. BMJ Leader, 5(3), 206–213. https://doi.org/10.1136/leader–2020–000360
Ma, X., & Xu, J. (2004). Determining the causal ordering between attitude toward mathematics and achievement in mathematics. American Journal of Education, 110(3), 256–280. https://doi.org/10.1086/383074
Memarpour, M., Fard, A. P., & Ghasemi, R. (2015). Evaluation of attitude to, knowledge of and barriers toward research among medical science students. Asia Pacific Family Medicine, 14(1), Article 1. https://doi.org/10.1186/s12930–015–0019–2
Northouse, P. G. (2021). Leadership: Theory and practice (9th ed.). SAGE publications.
Okoduwa, S. I. R., Abe, J. O., Samuel, B. I., Chris, A. O., Oladimeji, R. A., Idowu, O. O., & Okoduwa, U. J. (2018). Attitudes, perceptions, and barriers to research and publishing among research and teaching staff in a Nigerian research institute. Frontiers in Research Metrics and Analytics, 3, Article 26. https://doi.org/10.3389/frma.2018.00026
Osman, T. (2016). Medical students’ perceptions towards research at a Sudanese University. BMC Medical Education, 16(1), Article 253. https://doi.org/10.1186/s12909–016–0776–0
Özer, S. (2020). The predictiveness of attitude and motivation on achievement in ESP: The mediating role of anxiety. International Journal of Curriculum and Instruction, 12(2), 25-41.
Pallamparthy, S., & Basavareddy, A. (2019). Knowledge, attitude, practice, and barriers toward research among medical students: A cross–sectional questionnaire–based survey. Perspectives in Clinical Research, 10(2), 73.
Parker, S. M., Vona-Davis, L. C., & Mattes, M. D. (2021). Factors predictive of publication among medical students participating in school-sponsored research programs. Cureus, 13(9), e18176. https://doi.org/10.7759/cureus.18176
Peifer, C., Schönfeld, P., Wolters, G., Aust, F., & Margraf, J. (2020). Well done! Effects of positive feedback on perceived self-efficacy, flow and performance in a mental arithmetic task. Frontiers in Psychology,11, Article 1008. https://doi.org/10.3389/fpsyg.2020.01008
Pengpid, S., Peltzer, K., Puckpinyo, A., Tiraphat, S., Viripiromgool, S., Apidechkul, T., Sathirapanya, C., Leethongdee, S., Chompikul, J., & Mongkolchati, A. (2016). Knowledge, attitudes, and practices about tuberculosis and choice of communication channels in Thailand. Journal of Infection in Developing Countries, 10(7), 694-703. https://doi.org/10.3855/jidc.6963
Puljak, L. (2007). An overlooked source of physician–scientists. Journal of Investigative Medicine, 55(8), 402–405. https://doi.org/10.2310/6650.2007.00029
Rollnick, S., Butler, C. C., Kinnersley, P., Gregory, J., & Mash, B. (2010). Motivational interviewing. BMJ, 340, c1900. https://doi.org/10.1136/bmj.c1900
Rosenkranz, S. K., Wang, S., & Hu, W. (2015). Motivating medical students to do research: A mixed methods study using self-determination theory. BMC Medical Education, 15, Article 95. https://doi.org/10.1186/s12909-015-0379-1
Saini, M., Kumar, A., & Kaur, G. (2020). Research perception, motivation and attitude among undergraduate students: A factor analysis approach. Procedia Computer Science, 167, 185–192. https://doi.org/10.1016/j.procs.2020.03.210
Schellenberg, B. J. I., Gaudreau, P., & Bailis, D. S. (2022). Lay theories of obsessive passion and performance: It all depends on the bottom line. Personality and Individual Differences, 190, Article 111528. https://doi.org/10.1016/j.paid.2022.111528
Seitz, R. J., Paloutzian, R. F., & Angel, H.-F. (2017). Processes of believing: Where do they come from? What are they good for? F1000Research, 5, Article 2573. https://doi.org/10.12688/f1000research.9773.2
Simpson, R. D., & Oliver, J. S. (1990). A summary of major influences on attitude toward and achievement in science among adolescent students. Science Education, 74(1), 1–18. https://doi.org/10.1002/sce.3730740102
Sobczuk, P., Dziedziak, J., Bierezowicz, N., Kiziak, M., Znajdek, Z., Puchalska, L., Mirowska–Guzel, D., & Cudnoch–Jędrzejewska, A. (2022). Are medical students interested in research? – Students’ attitudes towards research. Annals of Medicine, 54(1), 1538–1547. https://doi.org/10.1080/07853890.2022.2076900
Taylor, D. C. M., & Hamdy, H. (2013). Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83. Medical Teacher, 35(11), e1561–e1572. https://doi.org/10.3109/0142159X.2013.828153
Tober, G. (2013). Motivational interviewing: Helping people change. Alcohol and Alcoholism, 48(3), 376–377. https://doi.org/10.1093/alcalc/agt010
Turner, J. E., Li, B., & Wei, M. (2021). Exploring effects of culture on students’ achievement motives and goals, self–efficacy, and willingness for public performances: The case of Chinese students’ speaking English in class. Learning and Individual Differences, 85, Article 101943. https://doi.org/10.1016/j.lindif.2020.101943
Valladares–Garrido, M. J., Mejia, C. R., Rojas–Alvarado, A. B., Araujo–Chumacero, M. M., Córdova–Agurto, J. S., Fiestas, J., Rojas–Vilar, F. J., & Culquichicón, C. (2022). Factors associated with producing a scientific publication during medical training: Evidence from a cross–sectional study of 40 medical schools in Latin America. F1000Research, 9, Article 1365. https://doi.org/10.12688/f1000research.26596.2
Wolf, E. J., Harrington, K. M., Clark, S. L., & Miller, M. W. (2013). Sample size requirements for structural equation models: An evaluation of power, bias, and solution propriety. Educational and Psychological Measurement, 76(6), 913–934. https://doi.org/10.1177/0013164413495237
Zhang, G., Wu, H., Xie, A., & Cheng, H. (2022). The association between medical student research engagement with learning outcomes. Medical Education Online, 27(1), Article 2100039. https://doi.org/10.1080/10872981.2022.2100039
*Anupong Kantiwong
317 Ratchawithi Rd,
Thung Phaya Thai,
Ratchathewi, Bangkok 10400
+66909838338
E-mail: anupongpcm31@gmail.com
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









