How do factors in fixed clinical teams affect informal learning among Emergency Medicine Residents
Submitted: 28 July 2022
Accepted: 12 October 2022
Published online: 3 January, TAPS 2023, 8(1), 25-32
https://doi.org/10.29060/TAPS.2023-8-1/OA2850
Choon Peng Jeremy Wee1, Mingwei Ng1 & Pim W. Teunissen2
1Department of Emergency Medicine, Singapore General Hospital, Singapore; 2School of Health Professions Education (SHE), Faculty of Health Medicine and Life Sciences, Maastricht University, Maastricht, The Netherlands
Abstract
Introduction: This study was performed to understand how fixed clinical teams affected informal learning in Emergency Medicine Residents. Better understanding the effects of team dynamics on informal learning may help to optimise learning and improve performance.
Methods: From 8th February 2020 till 27th September 2020, the Singapore General Hospital Emergency Department adopted a fixed team system. Zoom interviews were carried out amongst Emergency Medicine Residents who worked in the fixed team system using a semi-structured iterative interview guide. A qualitative content analysis was used for this exploratory study. The interviews were transcribed verbatim, anonymised and coding via template analysis performed. Data collection and analysis were performed until data sufficiency.
Results: The themes identified centred around relationship dynamics, team composition and motivation for learning. The first was how improved relationships led to improved trust, communications and camaraderie among team members. This improved peer learning and clinical supervision and provided a more personalised learning experience. A balanced team composition allowed learners to be exposed to experts in various subspecialties. Finally, there was an initial increase in motivation, followed by a decrease with time.
Conclusion: In postgraduate medical education, working in a fixed team system with balanced members had positive effects on informal learning by strengthening relationships and communications.
Keywords: Informal Learning, Workplace Learning, Fixed Teams, Medical Education, Postgraduate
Practice Highlights
- Fixed teams can strengthen relationships between members through better trust, familiarity and communication.
- A balanced fixed team with members having different areas of expertise allows a variety of perspectives.
- Rotation of team members may achieve a balance between the stronger relationship and familiarity of the members of fixed teams and the greater variance in perspectives from a non-fixed team system.
I. INTRODUCTION
Fixed teams (FT) and non-fixed teams (NFT) exist in medicine because of differing service requirements and manpower resources. Examples of FTs can exist in ward round teams and operating surgical teams (Eddy et al., 2016; Stepaniak et al., 2012) where personnel stay within the same work team for long periods. In other areas of healthcare like the Emergency Departments (ED), a NFT system is usually employed where teams are formed according to the personnel rostered to work on that shift and team members change every shift. This allows a more flexible system for the team members as they can request off days and leave according to their personal schedule and yet allows for 24-hour coverage in the ED.
High levels of performance are required of medical teams, both fixed and non-fixed, to achieve good patient outcomes. Therefore, team members should learn how to work effectively together to deliver the best patient care. There are studies, both within healthcare and other industries, which showed mixed results when FT were compared with NFT with regards to team performance. A systematic review on minimal invasive surgical teams found that the FTs had better teamwork and had reduced rates of technical mistakes compared to NFTs (Gjeraa et al., 2016). However, an aviation study showed that FTs made more minor errors compared to NFTs due to FT members being too familiar with each other and overlooking errors (Barker et al., 1996). Although it is unclear how transferable specific research findings from non-healthcare domains are, what is clear is that FTs and NFTs are different in the way teams were formed and the amount of time team members spend working together. There is a lack of understanding if and how these differences affect the way learning takes place in FT and NFTs; which could translate to the performance of the team and its members.
Workplace learning occurs through informal learning by experiencing work challenges and via interpersonal relationships. Informal learning can be supported through learner engagement by encouraging active participation in work activities and aligning learners’ interests with that of the organisation’s objectives towards improving the individuals’ and organisation’s capabilities (Billett, 2007). Informal learning is now widely accepted as a form of workplace learning that occurs out of a formal planned teaching program. It usually occurs during work activities which are not primarily aimed towards education, with learning objectives not planned beforehand (Callanan et al., 2011; Rogoff et al., 2016; Watkins et al., 2018). Although informal learning had been studied, there are very few studies looking at how being in FTs affects informal learning. A review on the involvement of employees in workplace learning (Kyndt & Baert, 2013) revealed that there was a paucity of literature on whether any team system improves the involvement of employees in informal learning. Thus, it remains to be studied what effects working in a FT system has on informal learning especially of the more junior team members.
An integrative literature review on informal learning found that some of the important components of informal learning within members of a team and between teams included interpersonal relationships, feedback, networking and leadership (Jeong et al., 2018). Therefore, there may be differences in interpersonal relationships and feedback between the different team systems. It is known that good interpersonal relationships include good supervisor and peer support and both affect whether what is learnt is applied at the workplace (Burke & Hutchins, 2016), there was little published data on whether supervisor and peer support or even the supervisory relationship were affected by the amount of time spent together. Within some healthcare systems both FTs and NFTs consists of members with varying levels of experience, differing expertise and roles. In a FT, the learners are only supervised by supervisors within that team; therefore, each learner’s supervised time is divided within a small group of supervisors as compared to a NFT system where each learner’s supervised time is spread amongst a larger number of supervisors. Thus, despite this increased time spent together in a FT, it is not clear if working in a FT impacts supervisory or interpersonal relationship.
Having a good trusted learner-supervisor relationship can result in the establishment of an “Educational Alliance” (Telio et al., 2015). This is because feedback from a credible trusted source was more readily accepted and feedback is another important component of effective informal learning within a team (Jeong et al., 2018).
Furthermore, a study among social work students and their supervisors in a rotational placement model, found that the longer the amount of time they spent with each other the greater the trust between them (Vassos et al., 2017). On the other hand, being in a FT could restrict networking and socialisation to a smaller group of people as contact with other teams’ members could be reduced however it is not known how this could affect informal learning.
Understanding how informal learning takes place within FT and NFT may allow optimisation of learning within each and perhaps even configure teams to enhance learning and thus ultimately improve performance. Our study aimed to fill this gap in the literature by exploring how fixed clinical teams affected the experience of informal learning for Emergency Medicine (EM) Residents. By doing so we hope to understand how informal learning can be supported via the appropriate implementation of team systems especially where high performance is expected from the teams.
II. METHODS
To study how being in fixed clinical teams affected the experience of informal learning for EM Residents we conducted an exploratory qualitative study based on a constructivism research paradigm using content analysis of individual interviews. This is because informal learning could not be quantified with specific learning outcomes.
A. Setting
EDs teams manage a large number of critically ill patients who may need time sensitive interventions. These teams would comprise of experienced Emergency Physicians (EPs) and more junior Medical Officers (MOs) and Residents. The Residents are postgraduate doctors who are training to graduate as EPs; therefore, informal workplace learning is a crucial part of their training. Hence the residents would be good study subjects to investigate the effect of team systems on informal learning.
The Singapore General Hospital (SGH) ED functioned via NFTs where the composition and number of members in the team differed with each 8 hour shifts accordingly to the anticipated patient load. The COVID-19 pandemic provided a naturalistic setting where the effect of a FT system can be compared to a NFT system which had existed before hand. After COVID-19 was declared a pandemic by the World Health Organisation (WHO) on the 11th March 2020 (World Health Organisation, 2020). There was an emphasis on infection control to contain the pandemic. Many countries had instituted social distancing measures which included curfew-like measures and travel restrictions (Lake, 2020). Similarly, the Singapore government had instituted legislative measures to limit face-to-face interactions. In the ED of SGH, measures were put in place to limit the spread of COVID-19.
Thus, from 8th February till 27th September 2020, as part of infection control measures, doctors were organised into 5 FTs, each having between 5-7 Consultants, 3-5 EM Senior Residents, 2-3 EM Junior Residents and 7-9 non-EM Medical Officers (MO) (Liu et al., 2020; Quah et al., 2020). The Senior Emergency Physicians (SEPs) consisted of certified specialists in EM (Associate Consultants, Consultants and Senior Consultants); they played supervisory and educational roles to the junior doctors (JD) which included MOs, Junior Residents and Senior Residents. Each FT worked 12-hour shifts. Interactions between teams were kept to a minimum and members from different teams were not allowed to mingle. Thus, the residents were only supervised by their team’s SEPs. Informal learning would now occur within these FTs.
Formal learning was converted to a remote online platform because of infection control measures. Lectures and tutorials were held and recorded using software which enabled online asynchronous access e.g. Zoom (Zoom, 2016) as not all residents could be given protected learning time together. Sessions which could not be transferred onto an online platform (e.g. hands on simulation and procedure skills training) were cancelled. Formal summative examinations were also cancelled.
B. Interviews
Interviews were conducted and recorded via Zoom (Zoom, 2016) to maintain social distancing. The primary investigator performed 11 interviews and a coinvestigator performed the remaining 4 out of a total of 15 interviews. A semi-structured iterative interview guide was developed based on Eraut’s typology on informal learning which included team activities, tasks and enabling/disabling factors (Eraut, 2010) was used, and the interviews were audio-recorded and transcribed verbatim and anonymised. The interviews allowed positive and negative aspects to be explored and being semi structured the questions asked varied according to the interviewees’ responses. This helped to focus the interviewees to what informal learning was with examples when it could occur within team activities. The guide was iteratively amended with each interview to enhance clarity which helped to obtain more in-depth data in later interviews.
C. Participants
Twenty-four ED residents were working in the FT system in the ED of SGH during COVID-19. Fifteen were Junior Residents and 9 were Senior Residents. Purposive sampling was carried out with at least two Residents from each team being sampled. This is to ensure that there was good representation for all of the fixed clinical teams. All 24 residents were invited to participate via email and WhatsApp messaging platform with written consent being obtained. Fifteen individual interviews were conducted before data sufficiency was achieved where no new data would change the outcome of the study, thus no further interviews were conducted beyond data sufficiency (Varpio et al., 2017). Eleven interviewees were Junior Residents (4 females and 7 males) and 4 were Senior Residents (3 females and 1 male).
D. Data Analysis
Data analysis was performed via template analysis by the primary and coinvestigator independently (Brooks et al., 2015). Eraut’s typology developed from his research on informal learning was used as a priori themes in the initial coding template (Eraut, 2010). Coding template modifications were made as the analysis of the transcripts continued. Themes were categorised into hierarchical clusters and relationships between them were studied and defined. After final modifications, the coding template was applied to the entire data set. Coding themes were compared and discussed between the primary investigator and the coinvestigator until consensus was reached.
E. Ethics
Waiver for approval was granted by the Singhealth Institutional Ethics Board. The primary investigator was a core faculty within the Singhealth Emergency Medicine Residency Program and although the interview was conducted among EM residents the primary investigator did not conduct the interviews when the interviewees were from the same team as the primary investigator. These were conducted by the coinvestigator. The coinvestigator was an EM Senior Resident who was not involved in the FT system. A reflexivity diary was kept, and peer debrief was done.
III. RESULTS
Three main themes emerged on how working in FTs affected informal learning amongst our participants (Figure 1). These included changes in relationship dynamics between members, effect of FT composition on informal learning of the participants and influence on motivation.
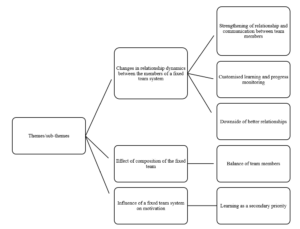
Figure 1. Themes and sub-themes
Theme 1: Changes in Relationship Dynamics between FT Members
From the interviews, the participants felt that the FT system resulted in more familiarity, trust, teamwork and improved communications between team members including SEPs, Residents and MOs. Interviewees felt that this strengthened the relationship dynamics between FT members as compared to a NFT. This meant that FT members were able to coordinate and exchange information better. It led to an increase in familiarity in knowing each member’s style of practice and way of thinking. The team members could understand each other better and how they reasoned.
The strengthened relationship between residents and SEPs changed with dynamics. Having a “closer rapport” and “deeper bond” allowed the residents to “tag along” with SEPs “more often” and gave the residents more insight as to why the SEPs behaved in a certain way as to “how they had practiced medicine” and the rationale behind each step was “more easily communicated to the residents who were tagging along” (Resident A), resulting in residents having a deeper understanding of why things were done in addition to how things were done. This strengthened relationship was also present between the residents and their peers. Therefore, peer learning improved within the FTs as junior residents reported feeling less reservation in asking each other questions.
Resident D felt that peer learning was better within FTs because of the improved relationship, there were less reservations which had prevented him from asking his peers questions in a NFT setting.
He elaborated:
“Fixed team [was] definitely better for peer learning. For the same reasons, because you know each other better, you’re more familiar. We don’t only talk to each other about work… after a while, when you go for meals together… or rather like resting together and no cases around you sit and talk. So there’s a lot more familiarity with the person you’re working with, and… you’re just more comfortable with asking questions… you don’t feel like this is somebody who’s going to judge you if [you] asked a stupid question”
This was not just amongst the residents but also with SEPs. Resident G felt that it was easier for the residents to speak to the SEPs because of familiarity and resulted in less workplace stress:
“Over the time as we knew each other better … the workplace stress was much lower… so I could… work with less stress at workplace… Because if you didn’t really know the consultant you tend to be afraid to talk to them; then of course your stress levels will be higher. But if you know that consultant and you know what kind of person, he or she is then you could be more comfortable to talk to them…”
“…It is more comfortable to… approach the senior because you know every day… we have a fixed team so naturally we feel that our relationship is closer…”
“… so, I won’t be too afraid to speak out or to talk to them to discuss with them.”
Contributing to additional ways of informal learning, communication within FTs even during work took on a more “friendly [and] social” form with greater congeniality and via more “communication platforms” (WhatsApp and Tiger Text) which continued even “outside of work” (Resident H). These platforms were also used as learning tools to facilitate case discussions, share learning points and experiences. This was not previously present in the NFTs. The residents felt that learning was more customised because of the change in relationship dynamics. In FTs, there was closer supervision of residents by SEPs. The residents “spent more time” with the same group of supervisors, thus the supervisors were able to better “assess both strengths, weaknesses and address any particular loopholes” of the residents (Resident A).
However, there were some adverse effects of this change in relationship dynamics. Some residents felt that with a closer relationship between team members, supervisors sometimes were more tolerant of the learners’ shortcomings and be less likely to point it out because of not wanting to affect the relationship. This closer relationship could result in residents taking “shortcuts” and “flying under the radar” because they knew the SEPs could tolerate or would not scrutinise the learners closely once “trust” was established (Resident L). Resident H gave an example of how familiarity could lead to less critical thinking by the learner:
“If… the senior always does like… [Rapid Sequence Intubation] … even though I question the first time I saw him do that… subsequently … every time I work with him I will do [it] this way. I won’t really think does the patient really need this way [of management] or will the patient benefit in a different way… if you are working with different bosses then every case you need to restart your thinking…”
Theme 2: Effect of Composition of the FT
All interviewees felt that the composition of the FT had affected informal learning, and that having a balanced team in terms of a wide range of years of practice amongst both the SEPs as well as the JDs would help improve informal learning. Having a team where the JDs were of differing seniorities of practice could help with peer learning because the senior ones could help the junior ones more. This also applied to the SEPs as that provided a wider perspective to clinical issues due to having different clinical experience and expertise in different subspecialties. Furthermore, if the JDs in a FT were of a similar level of practice, Resident C expressed that they could be “competing with each other for cases and procedures” which adversely affected informal learning with fewer opportunities to perform procedures. In a NFT the members would be constantly changing and it would be unlikely its JD would be always of the same level of practice.
The interviewees expressed concern that within a FT system that, although residents had close contact with a fixed group of supervisors, they lacked contact with the other teams’ SEPs. Many residents felt that this had adversely impacted informal learning because the SEPs were experts in different subspecialties (e.g., Trauma, Toxicology, Ultrasound, etc). By not interacting with many SEPs, residents were unable to learn from them. Furthermore, different supervisors had different perspectives and approaches to patients which the residents may not be exposed to if they were not in the same team as these seniors. However, this was mitigated by having a team with a balanced variation in the areas of specialty of the seniors. Resident F summarised this:
“…a team with… people from different seniorities are essential… (even) juniors can teach seniors… the way that my team was composed… it was a good mix… there are people from different… specialties… from different seniorities even within the juniors … like first posting to… [senior post graduate years]… offers different perspectives, learning of different things… people from different [subspecialties] can offer insight into the systems-based learning or component from other parts of the institution…”
Theme 3: Influence of a FT System on Motivation
Many residents felt that having FTs increased their motivation to learn. This resulted from their supervisors being able to inspire them and follow up with their learning progress more closely. Resident M was motivated to learn because his “friends (FT members) were very motivating” and “enthusiastic”; this encouraged him to learn more. Furthermore, resident C felt more motivated to learn in a FT because he “always sees the same senior” and this more frequent contact results in him being “more likely to take their feedback and opinion more seriously and work harder”
However, “after some time everyone is comfortable with each other” and some participants feared that their motivation “might go down” (Resident N). This was because there was a feeling of complacency as time went on within a FT, hence the motivation to learn started to dwindle after an initial increase.
Other reasons for this decline were related to COVID-19, the focus was more on facing the threat rather than learning and the priority to learn was secondary. The motivation to learn “was a bit less” as “the mood was more to survive than to learn”; Resident L was “less driven to learn” because there was a “general bleakness in the whole situation of [COVID-19] which made his “inner desire to learn… wane a bit”
IV. DISCUSSION
This study explored how working in fixed clinical teams affected informal learning for EM Residents. There are many pros and cons to fixed team rostering however the focus of this study is on informal learning. The findings highlighted the importance of having a balanced team composition where team members were able to establish trust and a strong bidirectional relationship because of the longer time spent working together. Motivation to learn increased initially; however after some time, some felt a decrease. This was consistent with prior work which highlighted team dynamics and commitment and that feedback which was given often and in a socially interactive environment were factors which helped to enable effective work-based learning (Attenborough et al., 2019; Jeong et al., 2018; Kyndt et al., 2016). Unlike in Attenborough’s work where team leadership was one of the factors identified; our respondents did not mention the effect of team leadership on informal learning. Their focus was more on the relationships between the different team members. From this study the predominant factors which positively affected informal learning included teamwork, collaborative task performance, where good communication was needed between different people, and personal development especially in building interpersonal relationships and group decision making.
Limited studies were done on how FTs affect informal learning. Our study found that FTs resulted in more (informal) communication channels (e.g. WhatsApp) being formed which was not present in NFTs, resulting in more learning activities including sharing ideas, resources and experiences. These sharing activities were some of the major forms of informal learning activities identified in the literature (Lohman, 2006). FTs resulted in open communication and quality feedback which was well received, and were found to be beneficial towards informal learning (Jeong et al., 2018). Our study showed that working in a FTs led to more customised learning. Findings of improved communications and strengthened relationships in a bidirectional manner involving teacher and learner alike, supports a shift from a predominantly teacher to learner type of dynamics to a team learning dynamics where all team members can learn with and from one another. This is important because informal learning takes place effectively when learning from past mistakes and feedback exchange occurs, involving both cognitive and social interactions (Jeong et al., 2018).
FTs had negative effects on informal learning as well. Familiarity resulted in supervisors being more tolerant of shortcomings and FTs limited learners’ contact with other teams’ supervisors and adversely affected informal learning. This was because informal learning also takes place when there is sharing of ideas, expertise and experience (Lohman, 2006) and limiting the number of supervisors limits the variance of shared viewpoints.
Our study has limitations. Firstly, interviewee recall bias was possible because 6 months had passed after the FT system was stopped before the interviews. Therefore, some details may not have been accurately recalled given this period which could affect the trustworthiness of results. Secondly, the participants were likely to be comparing their experiences in the FT system during COVID-19 to a NFT system without a pandemic. Thus, some of the experienced changes may be because of the pandemic rather than purely due to the FT system. Thirdly, there are many pros and cons to FTs however the focus of this study is on informal learning thus other factors not investigated with this study may affect the feasibility of FT. Lastly there could be power differential effects between the interviewers and the interviewees because the interviewers performed supervisory and roles to the residents. However, to mitigate this, a reflexivity diary was kept, and peer debrief between the two interviewers was performed. Furthermore, the interviewers did not interview members who had been in the same team as them.
V. CONCLUSION
In conclusion, FTs impact informal learning by building strong relationships with improved team communications and adding a social dimension for learning. A balance of team members as well as rotating the residents across different FTs may be beneficial for improving informal learning for EM Residents.
Notes on Contributors
Dr Wee Choon Peng Jeremy submitted the CIRB application, (with the help of the last author) conceptualised the study and its design. He performed the literature review, recruited and interviewed the participants, collected and transcribed the data, performed the thematic analysis of the data and wrote the manuscript.
Dr Ng Mingwei helped to recruit and interview some of the participants, transcribed and collected the data. Dr Ng helped perform the thematic analysis of the data and helped edit the manuscript.
Prof. Dr. Pim Teunissen was central to the conceptualisation of the study, advised on the design of the study and gave critical feedback to the writing of the manuscript and edited the manuscript extensively
All the authors have read and approved the final manuscript.
Ethical Approval
We have included the letter for waiver of CIRB via email. Ethics approval for waiver of written informed consent was obtained from the Singhealth Institutional Review Board (CIRB Ref: 2020/3114).
Data Availability
As the data set is qualitative in nature, we are not able to upload that in any public repository.
Funding
There is no funding for this paper/study.
Declaration of Interest
The authors report there are no competing interests to declare.
References
Attenborough, J., Abbott, S., Brook, J., & Knight, R. A. (2019). Everywhere and nowhere: Work-based learning in healthcare education. Nurse Education in Practice, 36, 132-138. https://doi.org/10.1016/j.nepr.2019.03.004
Barker, J. M., Clothier, C. C., Woody, J. R., McKinney, E. H., Jr., & Brown, J. L. (1996). Crew resource management: A simulator study comparing fixed versus formed aircrews. Aviation, Space, and Environmental Medicine, 67(1), 3-7.
Billett, S. (2007). Constituting the workplace curriculum. Journal of Curriculum Studies, 38(1), 31-48. https://doi.org/10.1080/00220270500153781
Brooks, J., McCluskey, S., Turley, E., & King, N. (2015). The utility of template analysis in qualitative psychology research. Qualitative Research in Psychology, 12(2), 202-222. https://doi.org/10.1080/14780887.2014.955224
Burke, L. A., & Hutchins, H. M. (2016). Training transfer: An integrative literature review. Human Resource Development Review, 6(3), 263-296. https://doi.org/10.1177/1534484307303035
Callanan, M., Cervantes, C., & Loomis, M. (2011). Informal learning. Wiley Interdisciplinary Reviews Cognitive Science, 2(6), 646-655. https://doi.org/10.1002/wcs.143
Eddy, K., Jordan, Z., & Stephenson, M. (2016). Health professionals’ experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. JBI Database of Systematic Reviews Implementation Reports, 14(4), 96-137. https://doi.org/10.11124/JBISRIR-2016-1843
Eraut, M. (2010). Informal learning in the workplace. Studies in continuing education, 26(2), 247-273. https://doi.org/10.1080/158037042000225245
Gjeraa, K., Spanager, L., Konge, L., Petersen, R. H., & Ostergaard, D. (2016). Non-technical skills in minimally invasive surgery teams: A systematic review, Surgical Endoscopy, 30(12), 5185-5199. https://doi.org/10.1007/s00464-016-4890-1
Jeong, S., Han, S. J., Lee, J., Sunalai, S., & Yoon, S. W. (2018). Integrative literature review on informal learning: Antecedents, conceptualizations, and future directions. Human Resource Development Review, 17(2), 128-152. https://doi.org/10.1177/1534484318772242
Kyndt, E., & Baert, H. (2013). Antecedents of employees’ involvement in work-related learning. Review of Educational Research, 83(2), 273-313. https://doi.org/10.3102/0034654313478021
Kyndt, E., Vermeire, E., & Cabus, S. (2016). Informal workplace learning among nurses. Journal of Workplace Learning, 28(7), 435-450. https://doi.org/10.1108/JWL-06-2015-0052
Lake, M. A. (2020). What we know so far: COVID-19 current clinical knowledge and research. Clinical Medicine, 20(2), 124-127. https://doi.org/10.7861/clinmed.2019-coron
Liu, Z., Teo, T. L., Lim, M. J., Nadarajan, G. D., Segaram, S. S. C., Thangarajoo, S., Wee, L. E., Wee, J. C. P., & Tan, K. B. K. (2020). Dynamic emergency department response to the evolving COVID-19 pandemic: The experience of a tertiary hospital in Singapore. Journal of the American College of Emergency Physicians Open, 1(6),1395-1403. https://doi.org/10.1002/emp2.12264
Lohman, M. C. (2006). Factors influencing teachers’ engagement in informal learning activities. Journal of Workplace Learning, 18(3), 141-156. https://doi.org/10.1108/13665620610654577
Quah, L. J. J., Tan, B. K. K., Fua, T. P., Wee, C. P. J., Lim, C. S., Nadarajan, G., Zakaria, N. D., Chan, S. J., Wan, P. W., Teo, L. T., Chua, Y. Y., Wong, E., & Venkataraman, A. (2020). Reorganising the emergency department to manage the COVID-19 outbreak. International Journal of Emergency Medicine, 13(1), Article 32. https://doi.org/10.1186/s12245-020-00294-w
Rogoff, B., Callanan, M., Gutiérrez, K. D., & Erickson, F. (2016). The organization of informal learning. Review of Research in Education, 40(1), 356-401. https://doi.org/10.3102/0091732×16680994
Stepaniak, P. S., Heij, C., Buise, M. P., Mannaerts, G. H., Smulders, J. F., & Nienhuijs, S. W. (2012). Bariatric surgery with operating room teams that stayed fixed during the day: A multicenter study analyzing the effects on patient outcomes, teamwork and safety climate, and procedure duration. Anesthesia and Analgesia, 115(6), 1384-1392. https://doi.org/10.1213/ANE.0b013e31826c7fa6
Telio, S., Ajjawi, R., & Regehr, G. (2015). The “Educational Alliance” as a framework for reconceptualizing feedback in medical education. Academic Medicine, 90(5), 609-614. https://doi.org/10.1097/ACM.0000000000000560
Varpio, L., Ajjawi, R., Monrouxe, L. V., O’Brien, B. C., & Rees, C. E. (2017). Shedding the cobra effect: Problematising thematic emergence, triangulation, saturation and member checking. Medical Education, 51(1), 40-50. https://doi.org/10.1111/medu.13124
Vassos, S., Harms, L., & Rose, D. (2017). Supervision and social work students: Relationships in a team-based rotation placement model. Social Work Education, 37(3), 328-341. https://doi.org/10.1080/02615479.2017.1406466
Watkins, K. E., Marsick, V. J., Wofford, M. G., & Ellinger, A. D. (2018). The evolving Marsick and Watkins (1990) theory of informal and incidental learning. New Directions for Adult and Continuing Education, 2018(159), 21-36. https://doi.org/10.1002/ace.20285
World Health Organisation. (2020). World Health Organisation emergencies press conference on coronavirus disease outbreak – 11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020
Zoom. (2016). Security guide. Zoom Video Communications Inc.
*Wee Choon Peng Jeremy
Outram Road,
Singapore 169608
Email: jeremy.wee.c.p@singhealth.com.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









