Impact of “just-in-time” simulation training for COVID-19 pandemic preparedness
Submitted: 6 April 2021
Accepted: 2 December 2021
Published online: 5 April, TAPS 2022, 7(2), 17-26
https://doi.org/10.29060/TAPS.2022-7-2/OA2510
Nicola Ngiam1,2, Kristy X Fu1,3 & Jacqueline SM Ong1,3
1Khoo Teck Puat- National University Children’s Medical Institute, National University Health System, Singapore; 2Centre for Healthcare Simulation, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 3Department of Paediatrics, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: Personal protection in aerosol-generating procedures is an important skill to safely deliver care to patients in the COVID-19 pandemic. This aim of this study was to evaluate the impact of “just-in-time” simulation training for airway management in a suspected COVID-19 patient.
Methods: This was a prospective mixed-method cohort study in a tertiary paediatric department. A mandatory “just-in-time” simulation training session for intubation of a suspected COVID-19 patient was conducted. Pre- and post-simulation questionnaires were administered. Participants were invited to attend focus group interviews to further delineate their experience. Quantitative and qualitative methods were employed to analyse the data.
Results: Thirty-three participants, including doctors, nurses and respiratory therapists attended the training. Self-confidence in intubation, managing and leading a resuscitation team and dealing with problems with intubation significantly improved. Simulation was valued for the experiential learning as well as for increasing confidence and awareness. Process improvement suggestions from both participants and trainers were raised. There was a small signal of skill translation to real life scenarios.
Conclusion: Simulation-based training is a useful tool for infectious disease outbreak preparedness. Further research will need to be done to determine the impact on actual clinical practice in pandemics.
Keywords: Simulation, COVID-19, Pandemic Preparedness, Training, Intubation
Practice Highlights
- The authors report their experience with “just-in-time” in situ simulation training for emergency preparedness in the face of an infectious disease outbreak.
- Simulation training was well received and improved the confidence as well as awareness of frontline staff in managing intubation and resuscitation in a suspected COVID-19 paediatric patient.
- Process improvement suggestions from participants and trainers was a useful by-product of the simulation training activity.
I. INTRODUCTION
Since the World Health Organization (WHO) declared the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) outbreak a public health emergency of international concern on 30 January 2020 (World Health Organization, 2020), the COVID-19 pandemic has now affected millions of people worldwide, with a wide range of case fatality rates amongst the 210 countries and territories affected (The Centre for Evidence-Based Medicine Nuffield Department of Primary Care Health Sciences University of Oxford, 2020). In Wuhan, China, one of the first epicentres of this international pandemic, out of 44672 confirmed cases of COVID-19, 1716 were healthcare workers (HCWs) (Wu & McGoogan, 2020). Of the confirmed cases among HCWs, 14.6% were classified as severe or critical, and 5 deaths were observed (The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, 2020). Early reports suggest that modes of transmission of SARS-CoV-2 include droplet and contact (via the fecal-oral route and fomites); airborne transmission may occur during aerosol-generating procedures (World Health Organization, 2020).
During the 2003 SARS-CoV outbreak, despite the presence of existing safety protocols, up to half of the SARS-CoV cases in some centers were HCWs as a result of transmission within hospital units (Booth et al., 2003). Critical care and emergency care providers are often involved in high-risk aerosol-generating procedures such as oronasal suctioning, bag-valve-mask ventilation, non-invasive positive pressure ventilation, and endotracheal intubation in patients with COVID-19 with respiratory failure, and so must be prepared (Caputo et al., 2006; Wax & Christian, 2020; Zuo et al., 2020). The challenge for providers would be to provide high-quality and timely care to infected patients, without compromising their own safety. Apart from having adequate supplies of personal protective equipment (PPE), a safe environment for HCWs requires the provision of up-to-date information regarding the disease, smooth dissemination of protocols, and easy accessibility to portals reinforcing education and training in infection control procedures. Lau et al. (2004) reported that HCWs who underwent more than 2 hours of training were far less likely to be infected with SARS-CoV during the 2003 SARS-CoV outbreak in Hong Kong. In addition to PPE training, we felt that a simulated airway management scenario in a suspected COVID-19 patient was a vital component of training in order for staff to experience the profound challenges of performing high risk aerosol-generating procedures while in PPE and in isolation facilities. During the recent 2014 to 2016 West Africa Ebola outbreak, Grillet et al. (2015) with the use of simulation, found that commonly performed procedures in the intensive care unit becomes more complicated, more stressful and less comfortable in appropriate PPE. We were fortunate to find a window of opportunity close to the beginning of the COVID-19 outbreak in Singapore to prepare our healthcare teams using “just-in-time” in-situ simulation. The main objective of this study was to evaluate the impact of this training on our resuscitation teams when managing a respiratory emergency of a suspected COVID-19 pediatric patient.
II. METHODS
This was a prospective mixed-method cohort study in a paediatric department of a tertiary university hospital. Residents were put through a mandatory “just-in-time” simulation training session to prepare them for intubation of a suspected COVID-19 patient. The doctors involved were senior paediatric residents who regularly manage emergencies on call. Nurses and respiratory therapists were rostered to participate whenever available on shift. Participants worked in teams of 5 to 6 to manage a simulation scenario involving a patient with bronchiolitis who was suspected to have COVID-19. Each team comprised of participants from each of the healthcare professional groups listed above. Actual personal protective equipment (PPE) including powered air-purifying respirators (PAPR) were used in the simulation. Participants received training in the use of PPE and PAPR prior to the simulation session. The simulation was conducted in-situ in the paediatric intensive care unit (PICU) using a SimBaby (Laerdal). The scenario used can be found in the appendix. Each group participated in one scenario. Each scenario lasted 30 to 40 minutes. The end point was successful intubation of the patient. There were 2 instructors (paediatric intensive care clinicians) present, one in the anteroom and one in the patient’s room. Debriefing was conducted as a group by both instructors immediately after every simulation. Each debriefing session lasted 30 to 45 minutes and focused on technical and non-technical skills.
Anonymous pre-simulation and post-simulation questionnaires were administered. Questions focused on confidence levels with managing intubation in a COVID-19 suspect patient, using the PAPR, and anxiety levels. Responses were rated on a Likert scale of 1 to 5. Quantitative data was analysed using Microsoft EXCEL, 2016. Pre and post responses on the Likert scale were analysed using the paired t-test.
After the simulation and debriefing, participants were invited via email to attend focus group interviews to gain better insight into their responses and attitudes towards the simulation sessions. The format and logistics of the interviews were included in a participant information sheet in the email. Participation was voluntary. We aimed for maximal representation from the various groups of healthcare professionals who participated in the simulation. A semi-structured interview was conducted by 2 researchers (NN, JO) in groups of 3 to 5 and interviews were audio-recorded. Two focus group interviews were conducted. Participants were asked questions regarding how they felt, what they learnt and what the benefits of the simulation experience were. Each interview lasted 30 to 40 minutes and were conducted in a quiet room in the PICU. Audio recordings were transcribed verbatim and anonymised at the point of transcription. Participants were only identified by role in the transcript.
Thematic analysis of the transcripts was performed by the 2 interviewers using an inductive approach. Each interviewer coded the data independently, after which both interviewers discussed the codes and generated common themes together. Data was reviewed for commonality in responses, degree of specificity (detailed explanation), and extensiveness (number of different people who had similar responses). Where there was disagreement, review of the data and existing literature was used for resolution. Descriptive summaries were developed for each theme, and participant quotes provided further evidence for interpretation and recommendations made.
This study was approved by the institutional review board (National Healthcare Group, Domain Specific Review Board, NHG DSRB Ref. 2020/00234) and waiver of consent was obtained.
III. RESULTS
A. Pre- and Post-Simulation Questionnaire Responses
A total of 33 participants took part in the training and completed the pre- and post-simulation questionnaires. There were 19 doctors, 12 nurses and 2 respiratory therapists. Confidence, as assessed by the questionnaire, increased significantly after the simulation in the areas of intubation, use of the PAPR, airway management in a COVID-suspect patient, leading a team and dealing with problems that arise during resuscitation (p < 0.05). Regarding anxiety over intubating a COVID-suspect patient, most participants were less anxious after the simulation (p < 0.05). Interestingly, on looking more closely at the responses, 9% (n=3) of participants were more anxious after the simulation than before they started. 42% (n=14) reported no change in their level of anxiety. Table 1 shows the mean scores of the questions asked in the pre- and post-simulation questionnaire.

Table 1: Pre- and post-simulation responses
After the simulation training, 96% of participants agreed or strongly agreed that they were more aware of who to call for help and how to communicate effectively when wearing PPE or PAPR while in an isolation room and 93% agreed or strongly agreed that they were more able to anticipate problems. All participants agreed that simulation training was useful in preparing to deal with a similar situation while on call and in fact, 23% disagreed or strongly disagreed that 1 simulation session was sufficient. Figure 1 illustrates the perceived effectiveness of simulation training by participants.
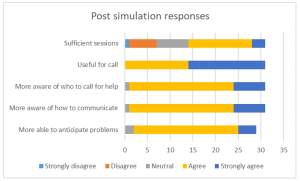
Figure 1: Post-simulation responses on effectiveness of simulation training
B. Focus Group Interviews
Eight participants agreed to focus group interviews, 4 doctors, 3 nurses and 1 respiratory therapist. Comments from the focus group interviews helped to further delineate the benefits and lessons learnt from this simulation exercise. Key benefits were grouped into the following themes:
1) Experiential learning: Participants commented that getting to put theory into practice during the simulation was key to understanding what to expect. Being able to practice before an actual patient encounter helped them to be more prepared. Even simple things like setting an intravenous cannula could not be accomplished with ease. Participants stated that they had to rethink the way that things needed to be done as how they were done previously would not work in this situation. This led to a paradigm shift in the clinical processes and also the application of knowledge. For example, a lesson learnt was that there is a lower threshold for intubation in COVID-19 patients. In the words of a participant about his experience:
“But the fact that you actually go through it, firstly you realize that it takes 3 times the length of the duration of what you would do, and the difficulties in communicating with the people around. So I thought that was the most…an awakening…. the most beneficial part.”
Participants appreciated that this was a complex scenario that was high stakes for the healthcare team as well as for the patient. Getting to practice this, even though it was likely to be an infrequent occurrence, helped with familiarity with protocols and equipment used. Participants also felt that more people should attend this training and that they needed more practice.
2) Increasing confidence: Participants felt that the simulation training was a timely intervention in light of the developing COVID-19 situation. This experience took away the “first-time” feeling and made the participants feel more comfortable with the protective equipment. This took away some of the anxiety and fear about their own safety and the safety of their COVID-19 patients. One participant stated that more practice in simulations may reduce the resistance to wearing the PAPR, which may in itself pose a safety issue if PAPRs are not used when required. They felt that this experience made them a more valuable member to the resuscitation team.
3) Increasing awareness: Participants appreciated the feedback and debriefing that came after the simulation. Experiencing the simulation made taught them to anticipate problems, plan ahead and to prioritize as resources were less accessible than usual. They developed insight into a possible “unconscious incompetence” as they expressed that if they had not gone through the simulation, they would not have known what they did not know and would be inappropriately confident in a real situation. Exploring resource management and considering aspects of waste reduction were thought to be beneficial for future encounters with similar situations. Some of our participants said:
“It really gives you…. the best kind of idea of what to expect in a real life scenario.”
“I would feel quite…. in a sense, bad for the patient that I was doing it for the first time on that patient. So I do feel that it is a responsible thing to do, as healthcare providers that we… that this was actually undertaken.”
“If we had not had this, I probably won’t even have that fear of how terrible it could have been……… But if I had not known, I would still be confident not knowing what I’m expecting.”
Some participants mentioned developing more empathy for colleagues caring for COVID-19 patients through this experience. However, one participant found herself more frustrated after going through the simulation as the experience of managing a resuscitation in this situation was worse than she had thought it would be.
4) Process improvement: In the focus group discussions, participants mentioned the need for process improvement that was discovered while encountering difficulties during the simulation scenario. Communication challenges were brought up multiple times and participants suggested making laminated signs for communication with staff outside the room when assistance was required, having pen, paper and drug labels in the room, as well as using intercoms or walkie-talkies for more efficient communication.
5) Translation: A couple of participants encountered a real subsequent clinical situation which required them to apply skills that they had learnt during the simulation training. The fact that they had gone through the training made them less anxious and more able to take control of the emergency situation. The respiratory therapist in the group expressed more confidence in the nurses that had gone through the simulation training when compared to those who had not when managing a COVID-19 patient. Participants also commented that the skills learnt could be translated to a different institution in the future and perhaps also to a different infective agent. Participants expressed the following:
“And so it would make you, I think… more valuable as a team member in providing care for a COVD patient or any other sort of respiratory pathogen X anywhere.”
“Because I observe that those nurses that attended the simulation, in the actual scenario or in the actual patient handling, they are more confident and competent in doing their PPE and flow of the sequence inside.”
“Because for me, for example, I actually had to initiate and help…coordinate initiation of ECMO for a COVID suspect patient and so I think if not for that…that mock… I would probably have been much more nervous and unsure.”
Key challenges encountered during the simulation were related to the simulation scenario and to the process of simulation itself. The most emphasised challenges encountered during the simulation were cognitive overload and communication barriers. Not only did the team have to deal with a deteriorating patient who was suspected to have COVID-19, they also had to deal with infection control protocols and the inherent challenges that it posed to the resuscitation process. As many tasks needed to be coordinated in a stressful situation, prioritisation was key. Communication barriers came in the form of restricted movement in and out of the isolation room, not being able to use their mobile devices, hearing impairment with the PAPR on and not being able to be heard clearly while wearing the N95 mask. Other challenges raised relating to the scenario were unfamiliarity with the safety equipment as it was not used frequently and having to wait a long time for orders to be carried out. An interesting challenge brought up was a tension between the patient’s safety or well-being and healthcare worker’s own safety. Healthcare professionals frequently put their patients first and in this unique situation, the need for donning personal protective equipment before entering the patient’s environment does not allow for as rapid a response to a deteriorating patient as they are used to:
“I feel like I need to go in as soon as possible but donning the PAPR takes some…. more time than I thought.”
Logistical challenges in planning for this simulation training included the availability and timely attendance of all frontline healthcare workers. With the developing crisis, healthcare professionals were kept busy with their clinical responsibilities, therefore this simulation training was seen as an unwelcome interruption. There was also a perceived resistance to participating by the nurses although the reasons are unclear.
Participants also commented on the design of this simulation training. Prior training in the process of intubation and use of PPE and PAPR were deemed necessary to optimize the benefits of this exercise. Participants appreciated that there were 2 trainers, 1 in the ante-room and 1 in the patient’s room, who were observing different processes and able to give valuable feedback during the debriefing. They also appreciated that the simulation exercise was done in-situ, and therefore was realistic in design.
Suggestions for improvement included providing a variety of clinical scenarios, training junior physicians so that the whole medical team is familiar with the processes, mimicking the typical manpower available on-call in the simulation exercise, and increasing the complexity of the scenarios to address resource allocation issues faced in a pandemic.
IV. DISCUSSION
With the development of the COVID-19 outbreak and patients requiring intensive care, our unit thought it would be imperative to train our frontline staff to be prepared to manage airway emergencies and to be able to resuscitate infected patients. Simulation provides a safe environment for mistakes to be made without compromising patient safety (Ziv et al., 2000). It also provides a platform for deliberate practice (Ericsson, 2004) and not allow for a chance clinical encounter to develop expertise in an area. Simulation has also been utilised in high consequence infectious outbreak training, resulting in improved self-efficacy, reduced anxiety and improved inter-professional teamwork (Marrs et al., 2019; O’Keeffe et al., 2016). As the consequences for patient and individual safety were high in the COVID-19 outbreak, we felt it was prudent to use simulation-based education as a platform for upskilling our staff.
Despite training in the use of personal protection equipment (PPE), including the powered air-purifying respirator (PAPR), Watson et al found that there was an inadequate adherence to the use of PPE and resuscitation guidelines in simulated cardiac arrest in paediatric influenza (H1N1) patients (Watson et al., 2011). Intensive care procedures have been found to be more difficult, stressful and uncomfortable when performed in PPE (Grillet et al., 2015). Simulation training has also been able to detect breaches in infection control procedures (Seet et al., 2009) and potentially improve compliance with infection prevention measures (Tan et al., 2021).
For the above reasons, healthcare professionals who worked in the paediatric intensive care unit were put through a mandatory simulation-based training session on airway management of a deteriorating patient who was suspected to have COVID-19 infection. An in-situ model was chosen as it could be used to evaluate system competence and identify latent conditions that predispose to medical error (Patterson et al., 2013). In this study, in situ simulation provided a means to identify areas for process improvement and knowledge gaps. It provided the ability to test the actual clinical care system, including equipment, processes, and staff response. This form of “just-in-time” training takes place in close proximity to the clinical encounter in a focused concise manner (Itoh et al., 2019). This provides the participants with contextually relevant hands-on experience in dealing with an impending low-frequency event before it actually happens. This has shown to improve confidence levels and clinical skills (Sam et al., 2012).
As expected, there was improvement in self-efficacy as shown in the improvement in pre- and post-simulation responses for all questions relating to management of the patient and clinical team. This has been shown in many previous studies using simulation as a methodology (McLaughlin et al., 2019; Secheresse et al., 2020). Evidence does suggest that clinicians have a limited ability for self-assessment of competence (Davis et al., 2006) and self-assessment. From the Kirkpatrick levels of evaluation, this would be a level 2 evaluation of knowledge, skills and attitudes (Kirkpatrick & Kirkpatrick, 2006). From the qualitative data, the benefits that were emphasised where related to experiential learning and increasing confidence as well as awareness. Kolb’s framework of experiential learning includes the phases of concrete experience and reflective observation (Kolb, 1984). These phases were evident in the simulation experience. Participants reflected that theoretical knowledge does not guarantee perfect execution in real life. The cognitive load of managing a high consequence, low incidence event along with the concomitant risk of exposure to a highly infectious agent makes clinical decision making harder. Although the participants underwent prior PPE training, they appreciated the opportunity to put it all into practice.
There was a definite signal for increased self-efficacy and confidence. This is seen in the literature on simulation-based healthcare education across disciplines (Bragard et al., 2018; Cohen et al., 2013; Fisher et al., 2011; Fouilloux et al., 2019). A study on influenza pandemic preparedness showed that simulation improved staff confidence and also demonstrated that many tasks and procedures took longer to complete with the implementation of guidelines (Phin et al., 2009). This was similarly evident in our participants as they became more aware of the challenges and the additional time needed for most resuscitative actions due to infection control requirements. Going through the simulated scenario and debriefing made them feel more prepared for an actual emergency. In addition, participants highlighted that the simulation experience alleviated anxiety as it successfully removed the “first-time” feeling for them, and felt that it was the responsible thing to do for healthcare workers in the midst a public health crisis. Lessons learnt by the participants included anticipatory planning, prioritisation and resource management. We had a small signal that the skills learnt translated to real life as one participant had a clinical encounter that required initiating extracorporeal life support in a patient with suspected COVID-19. She reported feeling relieved that she had the simulation experience before the real-life clinical encounter, and felt she was less nervous because of her prior stimulated experience. A respiratory therapist also observed that the nurses who he worked with in the PICU who had gone through the simulation seemed more confident and more aware of the necessary processes when intubating suspected COVID-19 patients.
An interesting phenomenon was the signal that there was an increase in anxiety levels after participants went through the simulation as seen in the pre- and post-simulation response. A possible explanation could be what participants brought up in the interviews about the simulation and debriefing revealing their “unconscious incompetence”. This made them more aware of the complexity and so increased their anxiety with dealing with intubation in a COVID-19 patient. Other studies in the literature generally report a reduction in anxiety after simulation (Bragard et al., 2019; Shrestha et al., 2019, 2020). This may not be a negative impact arising from the simulation experience itself as it may reflect increased awareness in an uncommon, yet stressful and complex clinical situation for our healthcare workers. Anxiety levels in frontline healthcare workers in a pandemic may also be due to other factors such as being at higher risk of exposure to COVID-19 at work and the possibility of bringing the infection home to their family (Holmes et al., 2020; Shanafelt et al., 2020).
Another benefit derived from running this simulation-based training is the process improvement suggestions made by the participants. This is a known benefit of simulation (Paige et al., 2018) and was utilised during the 2003 SARS-CoV outbreak (Abrahamson et al., 2005). The main challenge faced by participants during this scenario was the communication barrier which arose from not being able to communicate with personnel outside the room and the presence of the PPE and PAPR physically obstructing hearing and clarity of speech. Also, restriction of movement in and out of the patient’s room experienced during simulation highlighted the need to rethink resuscitation practices when dealing with COIVD patients. These systemic issues surfaced allowed us to brainstorm for practical solutions as a unit, and some have been implemented in our PICU. We have trialled the use of infant monitors as a 2-way communication device. Pre-packed resuscitation drug kits containing intravenous adrenaline and intravenous atropine as well as pre-packed intravenous cannulation disposables have been put in every isolation room so that these would be easily accessible in an emergency. As suggested by the participants, we have also extended the simulation training to include all junior doctors in the department, more nurses and all respiratory therapists in the PICU to facilitate better teamwork. We are also exploring the provision of a dedicated COVID-19 crash cart to minimise waste and prevent cross-contamination.
There are several limitations to this study. Firstly, the sample size is small and selection bias is possible due to the study design. Next, focus group interviews were conducted with a small subset of the participants who agreed to participate, and therefore our findings may not have been representative of the entire cohort. However, we are reassured by the fact that each healthcare professional group that took part in the simulation training was represented in the focus groups. As this simulation exercise was designed to be “just in time” training and we were limited by the urgency of the situation as well as the need to train as many staff in the shortest amount of time, we could only conduct a one-time simulation scenario specific to the highest risk procedure in resuscitating a suspected COVID-19 patient. We were therefore not able to assess the impact of this training on the subsequent performance of the participants either in another simulated scenario or a real life one.
V. CONCLUSION
Simulation-based training is a useful tool for infectious disease outbreak preparedness for the healthcare team. It improves confidence and awareness around managing emergencies while maintaining personal protection through deliberate practice in a safe environment. It also provides an opportunity for process improvement in a new and evolving pandemic situation. It was well-received by the participants and perhaps more sessions are needed for adequate practice. This is limited by the resource-intensive nature of in-situ simulation and the heavy clinical workload at this time of crisis. Further research will need to be done to determine if simulation-based training has a significant impact on actual clinical practice
Notes on Contributors
Nicola Ngiam conceptualised and designed the study, collected data, analysed and interpreted it, drafted the manuscript and approved the final version submitted.
Kristy X Fu did the background work and literature review, assisted in drafting the manuscript and critically revised the manuscript for important intellectual content and approved the final version submitted.
Jacqueline SM Ong designed the study, collected data, interpreted it, critically revised the manuscript for important intellectual content and approved the final version submitted.
Ethical Approval
Ethical approval has been granted by National Healthcare Group Domain Specific Review Board (Ref: NHG DSRB Ref. 2020/00234)
Data Availability
Transcripts from the interviews are confidential and the authors do not have consent to upload onto a repository. Data from questionnaires can be made available on request.
Acknowledgement
We would like to thank Dr Dimple Rajgor for helping with formatting, and submission of the manuscript for publication.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Interest
The Authors declare that there is no conflict of interest.
References
Abrahamson, S. D., Canzian, S., & Brunet, F. (2005). Using simulation for training and to change protocol during the outbreak of severe acute respiratory syndrome. Critical Care, 10(1), R3. https://doi.org/10.1186/cc3916
Booth, C. M., Matukas, L. M., Tomlinson, G. A., Rachlis, A. R., Rose, D. B., Dwosh, H. A., Walmsley, S. L., Mazzulli, T., Avendano, M., Derkach, P., Ephtimios, I. E., Kitai, I., Mederski, B. D., Shadowitz, S. B., Gold, W. L., Hawryluck, L. A., Rea, E., Chenkin, J. S., Cescon, D. W., Poutenan, S.M. & Detsky, A. S. (2003). Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA, 289(21), 2801-2809. https://doi.org/10.1001/jama.289.21.JOC30885
Bragard, I., Farhat, N., Seghaye, M.-C., Karam, O., Neuschwander, A., Shayan, Y., & Schumacher, K. (2019). Effectiveness of a high-fidelity simulation-based training program in managing cardiac arrhythmias in children: A randomized pilot study. Pediatric Emergency Care, 35(6), 412-418. https://doi.org/10.1097/PEC.0000000000000931
Bragard, I., Seghaye, M.-C., Farhat, N., Solowianiuk, M., Saliba, M., Etienne, A.-M., & Schumacher, K. (2018). Implementation of a 2-day simulation-based course to prepare medical graduates on their first year of residency. Pediatric Emergency Care, 34(12), 857-861. https://doi.org/10.1097/PEC.0000000000000930
Caputo, K., Byrick, R., Chapman, M., Orser, B., & Orser, B. (2006). Intubation of SARS patients: Infection and perspectives of healthcare workers. Canadian Journal of Anaesthesia, 53(2), 122-129. https://doi.org/10.1007/BF03021815
Cohen, E. R., Barsuk, J. H., Moazed, F., Caprio, T., Didwania, A., McGaghie, W. C., & Wayne, D. B. (2013). Making July safer: Simulation-based mastery learning during intern boot camp. Academic Medicine, 88(2), 233-239. https://doi.org/10.1097/ACM.0b013e31827bfc0a
Davis, D. A., Mazmanian, P. E., Fordis, M., Van Harrison, R., Thorpe, K. E., & Perrier, L. (2006). Accuracy of physician self-assessment compared with observed measures of competence: A systematic review. JAMA, 296(9), 1094-1102. https://doi.org/10.1001/jama.296.9.1094
Ericsson, K. A. (2004). Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Academic Medicine, 79(10), S70-S81. https://doi.org/10.1097/00001888-200410001-00022
Fisher, N., Eisen, L. A., Bayya, J. V., Dulu, A., Bernstein, P. S., Merkatz, I. R., & Goffman, D. (2011). Improved performance of maternal-fetal medicine staff after maternal cardiac arrest simulation-based training. American Journal of Obstetrics and Gynecology, 205(3), e1-e5. https://doi.org/10.1016/j.ajog.2011.06.012
Fouilloux, V., Gran, C., Guervilly, C., Breaud, J., El Louali, F., & Rostini, P. (2019). Impact of education and training course for ECMO patients based on high-fidelity simulation: A pilot study dedicated to ICU nurses. Perfusion, 34(1), 29-34. https://doi.org/10.1177/0267659118789824
Grillet, G., Marjanovic, N., Diverrez, J., Tattevin, P., Tadié, J., & L’Her, E. (2015). Intensive care medical procedures are more complicated, more stressful, and less comfortable with Ebola personal protective equipment: A simulation study. The Journal of Infection, 71(6), 703-706. https://doi.org/10.1016/j.jinf.2015.09.003
Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., Ballard, C., Christensen, H., Silver, R. C., & Everall, I. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry, 7(6), 547-560. https://doi.org/10.1016/S2215-0366(20)30168-1
Itoh, T., Lee-Jayaram, J., Fang, R., Hong, T., & Berg, B. (2019). Just-in-Time Training for Intraosseous Needle Placement and Defibrillator Use in a Pediatric Emergency Department. Pediatric Emergency Care, 35(10), 712-715. https://doi.org/10.1097/PEC.0000000000001516
Kirkpatrick, D., & Kirkpatrick, J. (2006). Evaluating training programs: The four levels (3rd ed.). Berrett-Koehler Publishers.
Kolb, D. (1984). The experiential learning theory of development. Experiential Learning: Experience as the Source of Learning and Development (pp. 132-160). Prentice Hall, Englewood Cliffs, NJ, 132-160.
Lau, J., Fung, K., Wong, T., Kim, J., Wong, E., Chung, S., Ho, D., Chan, L., Lui, S., & Cheng, A. (2004). SARS transmission among hospital workers in Hong Kong. Emerging Infectious Diseases, 10(2), 280-286. https://doi.org/10.3201/eid1002.030534
Marrs, R., Horsley, T. L., Hackbarth, D., & Landon, E. (2019). High consequence infectious diseases training using interprofessional simulation and TeamSTEPPS. American Journal of Infection Control, 48(6), 615-620. https://doi.org/10.1016/j.ajic.2019.10.007
McLaughlin, C., Barry, W., Barin, E., Kysh, L., Auerbach, M. A., Upperman, J. S., Burd, R. S., & Jensen, A. R. (2019). Multidisciplinary simulation-based team training for trauma resuscitation: A scoping review. Journal of Surgical Education, 76(6), 1669-1680. https://doi.org/10.1016/j.jsurg.2019.05.002
O’Keeffe, D., Bradley, D., Evans, L., Bustamante, N., Timmel, M., Akkineni, R., Mulloy, D., Goralnick, E., & Pozner, C. (2016). Ebola Emergency Preparedness: Simulation Training for Frontline Health Care Professionals. MedEdPORTAL, 12, 10433-10433. https://doi.org/10.15766/mep_2374-8265.10433
Paige, J. T., Fairbanks, R. J. T., & Gaba, D. M. (2018). Priorities related to improving healthcare safety through simulation. Simulation in Healthcare, 13(3S), S41-S50. https://doi.org/10.1097/SIH.0000000000000295
Patterson, M., Geis, G., Falcone, R., LeMaster, T., & Wears, R. (2013). In situ simulation: detection of safety threats and teamwork training in a high risk emergency department. BMJ Quality & Safety, 22(6), 468-477. https://doi.org/10.1136/bmjqs-2012-000942
Phin, N., Rylands, A., Allan, J., Edwards, C., Enstone, J., & Nguyen-Van-Tam, J. (2009). Personal protective equipment in an influenza pandemic: a UK simulation exercise. Journal of Hospital Infection, 71(1), 15-21. https://doi.org/10.1016/j.jhin.2008.09.005
Sam, J., Pierse, M., Al-Qahtani, A., & Cheng, A. (2012). Implementation and evaluation of a simulation curriculum for paediatric residency programs including just-in-time in situ mock codes. Paediatrics & Child Health, 17(2), e16-20. https://doi.org/10.1093/pch/17.2.e16
Secheresse, T., Pansu, P., & Lima, L. (2020). The impact of full-scale simulation training based on Kolb’s learning cycle on medical prehospital emergency teams: A multilevel assessment study. Simulation in Healthcare, 15(5), 335-340. https://doi.org/10.1097/SIH.0000000000000461
Seet, R., Lim, E., Oh, V., Ong, B., Goh, K., Fisher, D., Ho, K., & Yeoh, K. (2009). Readiness exercise to combat avian influenza. QJM : Monthly Journal of the Association of Physicians, 102(2), 133-137. https://doi.org/10.1093/qjmed/hcn159
Shanafelt, T., Ripp, J., & Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA, 323(21), 2133-2134. https://doi.org/10.1001/jama.2020.5893
Shrestha, R., Badyal, D., Shrestha, A., & Shrestha, A. (2020). In-situ simulation-based module to train interns in resuscitation skills during cardiac arrest. Advances in Medical education and Practice, 11, 271-285. https://doi.org/10.2147/AMEP.S246920
Shrestha, R., Shrestha, A. P., Shrestha, S. K., Basnet, S., & Pradhan, A. (2019). Interdisciplinary in situ simulation-based medical education in the emergency department of a teaching hospital in Nepal. International Journal of Emergency Medicine, 12(1), 19. https://doi.org/10.1186/s12245-019-0235-x
Tan, K. W., Ong, H. K., & Mok, U. S. (2021). Using simulation and inter-professional education to teach infection prevention during resuscitation. The Asia Pacific Scholar, 6(1), 93-108. https://doi.org/10.29060/TAPS.2021-6-1/OA2229
The Centre for Evidence-Based Medicine Nuffield Department of Primary Care Health Sciences University of Oxford. (2020). Global Covid-19 case fatality rates. https://www.cebm.net/covid-19/global-covid-19-case-fatality-rates/. Accessed April 26, 2020.
The Novel Coronavirus Pnuemonia Emergency Response Epidemiology Team. (2020). The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Weekly, 2(8), 113-122. https://doi.org/10.46234/ccdcw2020.032
Watson, C., Duval-Arnould, J., McCrory, M., Froz, S., Connors, C., Perl, T., & Hunt, E. (2011). Simulated pediatric resuscitation use for personal protective equipment adherence measurement and training during the 2009 influenza (H1N1) pandemic. The Joint Commission Journal on Quality and Patient Safety, 37(11), 515-523. https://doi.org/10.1016/S1553-7250(11)37066-3
Wax, R. S., & Christian, M. D. (2020). Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Canadian Journal of Anesthesia/Journal canadien d’anesthésie, 67(5), 568–576. https://doi.org/10.1007/s12630-020-01591-x
World Health Organization. (2020). Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019- nCoV). Retrieved 6 April, 2021, from https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
Wu, Z., & McGoogan, J. (2020). Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA, 323(13), 1239-1242. https://doi.org/10.1001/jama.2020.2648
Ziv, A., Small, S. D., & Wolpe, P. R. (2000). Patient safety and simulation-based medical education. Medical Teacher, 22(5), 489-495. https://doi.org/10.1080/01421590050110777
Zuo, M., Huang, Y., Ma, W., Xue, Z., Zhang, J., Gong, Y., & Che, L. (2020). Expert recommendations for tracheal intubation in critically ill patients with Noval Coronavirus Disease 2019. Chinese Medical Sciences Journal, 35(2), 105–109. https://doi.org/10.24920/003724
*Nicola Ngiam
Centre for Healthcare Simulation,
National University of Singapore,
14 Medical Dr,
Singapore 117599
Email: nicola_ngiam@nuhs.edu.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









