A SWOT analysis of medical school adaptations to COVID-19: A national survey of deans in Taiwan
Submitted: 5 July 2021
Accepted: 13 September 2021
Published online: 5 April, TAPS 2022, 7(2), 6-16
https://doi.org/10.29060/TAPS.2022-7-2/OA2654
Ming-Jung Ho1,2, Yu-Che Chang3,4,5 & Steven L. Kanter6
1Center for Innovations and Leadership in Education, Georgetown University Medical Center (CENTILE), Washington, D.C., United States; 2Department of Family Medicine, Georgetown University School of Medicine, Washington D.C., United States; 3Chang Gung Medical Education Research Centre (CG-MERC), Chang Gung Medical Foundation, Taoyuan, Taiwan; 4Chang Gung University College of Medicine, Taoyuan, Taiwan; 5Department of Emergency Medicine, Chang Gung Memorial Hospital, Linkou, Taoyuan, Taiwan; 6Association of Academic Health Centers, Washington, D.C., United States.
Abstract
Introduction: The COVID-19 pandemic forced medical schools worldwide to transition online. While there are ample reports about medical education adaptations to this crisis, there are limited studies evaluating the impact.
Methods: This study includes a case study of how Taiwanese medical school deans maintained in-person education during the COVID-19 pandemic. Additionally, it demonstrates how SWOT analyses can help medical educators reflect on adaptations during the COVID-19 pandemic and future crises. This study employed two online surveys and a semi-structured interview regarding curricular adaptations. Eligible participants were deans or associate deans of all medical schools in Taiwan.
Results: Through a SWOT analysis, this study identified Strengths as strong leadership, prior experience with SARS, and ability to promptly adapt curriculum; Weaknesses as lack of faculty confidence in online education, limited numbers of administrative staff, and inability to rapidly add new topics; Opportunities as centralised anti-epidemic policies, inter-institutional collaborations, and educational innovations; and Threats as concerns from parents, patients, and teaching hospitals. It is reported that the quality of education was maintained as students’ evaluations of courses, performances in written exams, clerkship supervisors’ assessments, national OSCE, and national board exams remained comparable to pre-COVID times. Strengths and Opportunities such as strong leadership and centralised anti-epidemic policies can overcome Weaknesses and Threats, such as lack of confidence in online education and familial pressure to suspend hospital-based education.
Conclusion: This study recommends that medical school leaders conduct SWOT analyses as early as possible to plan strategies to continue safe and quality medical education during COVID-19 and future crises.
Keywords: SWOT Analysis, Adaptation, Medical School, COVID-19, Pandemic, National Survey, Medical Education, Taiwan
Practice Highlights
- Medical school deans in Taiwan documented critical observations made during a global pandemic.
- SWOT analysis can help us reflect on medical education adaptations during the pandemic and crises.
- Strong leadership and centralised anti-epidemic policies can aid in overcoming weaknesses/threats.
- Schools can benefit from using SWOT analyses to plan for continuing education during emergent crises.
I. INTRODUCTION
The novel coronavirus disease 2019 (COVID-19) outbreak in Wuhan, China at the end of December 2019 evolved rapidly into a global pandemic and upended almost every aspect of our lives, including school closures across the world (UNICEF, 2021; Zhu et al., 2020). Medical schools are no exception (B. Choi et al., 2020; Harries et al., 2021). Almost all medical schools in the United States transitioned to online teaching by mid-March 2020 and tried to restart teaching on campuses and in hospitals safely in Fall 2020 (Frieden, 2020) . There is a growing literature on how to transition medical education online during the COVID-19 pandemic (Ahmed et al., 2020; Al-Balas et al., 2020; Journal of the Association of American Medical Colleges, 2021; Keegan & Bannister, 2021; Medical Education, 2020). Medical education associations also developed websites and offered webinars to share best practices and innovations focused on online education rather than in-person education (Association for Medical Education in Europe, 2020; Association of American Medical Colleges, 2021; International Association of Medical Science Educators, 2020). Most of the literature reflects the important perspectives of teachers and students with voices from medical school leadership and the forces impacting their decisions relatively limited (Abbas et al., 2020; Al-Balas et al., 2020; Compton et al., 2020; Gordon & Cleland, 2021; Lazarus et al., 2021; Soled et al., 2020). Furthermore, most of the publications are based on lessons learned from English-speaking countries. As non-English-speaking countries encountered COVID-19 and started to reopen medical schools earlier than English-speaking countries, lessons from non-English-speaking medical schools can be valuable to the global medical education community. This study addresses the above gaps in literature by surveying Taiwanese medical school deans on how they adapted their curricula and continued face-to-face medical education on campus and in hospitals amid this historical moment.
Located 81 miles from mainland China, and with over a hundred daily flights in between, Taiwan was predicted to have the second highest number of COVID-19 cases according to early modeling in January 2020 (Gardner, 2020). Having learnt a hard lesson from the severe acute respiratory syndrome (SARS) epidemic in 2003, the Taiwanese government, health system, general public, and medical educators were better prepared to respond to this new pandemic early and proactively (Wang et al., 2020). Before the first confirmed case in Taiwan, the Taiwan Centers for Disease Control began to monitor passengers returning from Wuhan, China, since on January 21, 2020 and set up the Central Epidemic Command Center to coordinate responses to COVID-19, including surveillance and testing, border control, community transmission control, medical system response, personal protective equipment (PPE) and other medical supplies stockpile and distribution, as well as health education and disinformation management (Taiwan Center for Disease Control, 2020).
In contrast to medical schools around world closing campus in the spring semester due to the COVID-19 pandemic, Taiwanese medical schools stayed open except for delaying the start of spring semester one or two weeks later than the originally scheduled date of February 17, 2020.
In addition to exploring how Taiwanese medical schools adapted their curriculum to continue on-campus and workplace-based education at the program level during the COVID-19 pandemic, this study addresses the gap in the literature regarding evaluation of these programmatic changes (Reid & Sam, 2021). This study employed a SWOT analysis (Ghazinoorya et al., 2011; Topor et al., 2018), a method widely used to analyse an organisation’s internal strengths and weaknesses, as well as external opportunities and threats in the environment to examine what medical education leaders critically consider in order to maintain in-person medical education amid the COVID-19 pandemic. This study surveyed and interviewed Taiwanese medical school deans in order to answer the following four research questions:
1. What curricular adaptations have been made in response to the COVID-19 pandemic?
2. What were the impacts of the curricular adaptations?
3. What were the strengths, weaknesses, opportunities, and threats of the curricular adaptations?
4. What are the lessons learned to be applied to the future?
II. METHODS
This study consists of two online surveys and a follow-up individual semi-structured interview. Eligible participants were deans or associate deans of all 13 medical schools in Taiwan. To encourage participation, we emailed invitations with information about study purpose, data confidentiality, and a weblink to the online survey. Participation was voluntary without incentives offered. Following the initial email, reminders were sent periodically. If the dean of a medical school was not available to complete the survey, we invited the associate dean to do so. We collected survey responses and conducted interviews about curricular adaptations between April 29 and May 18, 2020. A follow up survey on the impacts of curricular adaptation was conducted between August 27 and September 10. The online written surveys and follow-up semi-structured interviews were conducted in Chinese (written) and Mandarin (spoken) and translated to English by the first author (MJH). This study was approved as exempt by the Georgetown University Institutional Review Board (STUDY00002812). Since the study poses no greater than minimal risk to subjects, a waiver of written consent was granted, and verbal consent was obtained before data collection began. All methods were carried out in accordance with relevant guidelines and regulations.
A. Study Design
The survey questions were developed based on a review of relevant literature and consultations with international research collaborators in Italy, Japan and Korea, where similar surveys will be conducted. Open-ended survey questions can be found in Supplemental Digital Appendix 1.
In addition to the online survey, each participant was offered an opportunity to be interviewed by the first author (MJH) videoconference in the ensuing two weeks to provide further details about their survey responses. If a participant accepted the interview invitation, a semi-structured interview was conducted, in which the participant was prompted to elaborate on their answers in the surveys. Clarifying questions were asked for survey responses as needed. For example, a participant responded to a survey question by stating that an OSCE exam had been cancelled. During the ensuing interview, the interviewer asked “In the survey, you wrote that an OSCE was cancelled. What was the OSCE for? How did you make up for the cancelled OSCE?”
B. Data Analysis
The free text responses to the open-ended questions in the survey, as well as recordings of the interviews, were analysed by the researchers using a qualitative thematic analysis approach (Braun & Clarke, 2006). One researcher identified themes that emerged from the qualitative data; then, a second researcher determined if they agree or disagree with the analysis. For each point of disagreement, the two researchers discussed the data and reached consensus. Data analysis was initially inductive. After the themes emerged, we used a SWOT analysis framework to group themes into four categories: strengths internal to the institution, weaknesses internal to the institution, opportunities external to the institution, and threats external to the institution (Ghazinoorya et al., 2011; Topor et al., 2018).
III. RESULTS
All 13 medical schools in Taiwan completed the survey for a response rate of 100%. Eleven deans and two associate deans filled out the survey. Three deans and one associate dean agreed to participate in a follow-up interview by videoconference. Characteristics of the medical schools are listed in Table 1. In the first part of results, we will describe curricular adaptations and present themes with representative quotes of curricular adaptations in Table 2. Then Table 3 will summarise the SWOT analysis followed by descriptions of key themes in strengths, weaknesses, opportunities, and threats.
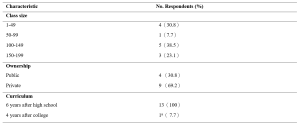
Table 1. Characteristics of Survey Schools
aOne medical school had both 6-year program for high school graduates and 4-year program for college graduates.
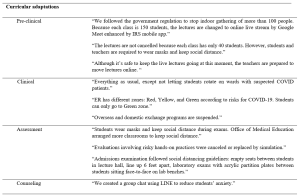
Table 2. Themes and quotes of curriculum adaptations
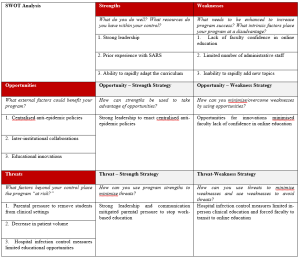
Table 3. SWOT Analysisb
b This table is created using the blank SWOT form from Topor et al.21
A. Curricular Adaptations
1) Pre-clinical curriculum adaptations:
Taiwanese medical schools rapidly adapted their curricula to comply with government policy on social distancing prohibiting indoor gatherings of more than 100 individuals. Whereas a school with a small student body and sufficient classroom capacity did not have to transition online, a school with a large student body and insufficient classroom capacity moved almost all pre-clinical classes online. Some schools went partially online, converting only lectures with more than 100 students to online learning and capping the number of students in the classroom, with live stream available for those not in the classroom. While schools adapted different modalities for lecture-based courses, all schools made efforts to keep laboratory courses face-to-face. Some schools shared how they adjusted laboratory sessions to maintain social distance, including simultaneously using more lab rooms or holding lab sessions in different time slots.
2) Clinical curriculum adaptations:
In contrast to approaches in the United States suspending clinical rotations in spring semester recommended by AAMC (Association of American Medical Colleges, 2021), all medical schools in Taiwan continued clinical rotations while protecting the safety of students. Several strategies were implemented rapidly: Orientation to clinical rotations articulated pandemic prevention and included online modules required by the hospital. Clinical students were provided with surgical masks. In the emergency room, students were given N95 respirators each day. Exposure to suspected and confirmed COVID-19 cases was avoided for students replacing rotations in specialties with high risk of COVID-19 exposure. To prevent cross infection, inter-institutional and overseas exchange programs were cancelled. Students rotated in only one of the affiliated hospitals. Social distancing is also mentioned in clinical rotation adjustments. Several respondents mentioned that the number of students in outpatient clinics, in classrooms, and in conferences was reduced. One school reported an increase of clinical teachers to meet social distancing demands.
3) Assessment adaptations:
Eight schools replied that they did not change the assessment of students by written examinations in classrooms but arranged empty seats between students to keep social distance and protected students from airborne droplet transmissions by requiring everyone to wear a mask. Some schools decreased the use of written exams in classrooms by substituting reports, reflections, online exams, online presentations, and other approaches. Some evaluations involving hands-on practices were cancelled or replaced by simulation. One school reported that their admission exams included tests in laboratories. To prevent face-to-face transmission of airborne droplets, transparent acrylic partitions were installed on the benches in front of each student.
B. Impact of curricular adaptations
Medical school deans tried to evaluate the impact of curricular adaptions by comparing student performance in the 2020 spring semester with previous years. Most deans reviewed the passing rate of courses and reported no statistical differences. They also reported monitoring students’ performances in national board exams in July and national OSCE clinical skills exam held before graduation. The deans were relieved to see that the national exam scores were comparable to previous years and felt that curricular adaptations didn’t impact student competencies negatively.
C. Strengths
The strengths of Taiwanese medical schools’ responses to COVID-19 can be summarised into three themes: strong leadership, prior experience with SARS, and ability to rapidly adapt the curriculum.
1) Strong leadership: The key strength most Taiwanese deans cited in their medical schools’ response to COVID-19 is the strong leadership in the early deployment of epidemic prevention measures. The guidelines from the Central Epidemic Command Center were implemented on each campus, including requiring students to wear masks, to maintain social distance, to monitor temperature and symptoms of COVID-19, and to quarantine international students in separate dormitory areas. Communication also was highlighted by respondents as manifesting strong leadership. Furthermore, two deans made videos in collaboration with students to promote anti-epidemic measures (Chang Gung University, 2020; Fu Jen Catholic University, 2020).
2) Prior experience with SARS: Another strength most respondents noted was the experience of SARS. When COVID-19 spread to Taiwan, most clinical teachers had experienced SARS and were able to share critical lessons to face new emerging infectious diseases with the younger generation. The experience of SARS also prepared medical educators to deal with professionalism and ethics issues such as distribution of limited medical resources. Many participants mentioned that SARS had a great impact on the medical education system in Taiwan because it exposed the lack of primary care workforce with medical school graduates entering specialty training directly after medical school. After SARS, a postgraduate year program was established with one year of required general medicine training prior to specialty training programs with the goal of producing more physicians competent in general medicine to respond to emergent infectious diseases.
3) Ability to rapidly adapt the curriculum: All schools reported rapid curricular adaptations when spring semester started one or two weeks later than the scheduled time. Different strategies were employed in pre-clinical and clinical curricula to prevent and control the spread of COVID-19 as described in 3.1 curricular adaptation.
D. Weaknesses
The weaknesses of Taiwanese medical schools’ responses to COVID-19 can be summarised into three themes: lack of faculty confidence in online education, limited number of administrative staff, and inability to rapidly add new topics.
1) Lack of faculty confidence in online education: All respondents mentioned online teaching as challenging to teachers. Many voiced concerns about the effectiveness of online learning and found assessment of online learning challenging. Online learning is also considered challenging to students. Some respondents mentioned that online learning requires self-directed learning, which is not a strength of Taiwanese students since didactic teaching and rote memorisation is the norm of the K-12 education system.
2) Limited number of administrative staff: In response to the question about weaknesses of their medical schools’ responses to the COVID-19 pandemic, administrative challenges were mentioned frequently. Although Taiwan did not experience high burdens of COVID-19, all schools were preparing for large-scale outbreaks with frequent scenario planning, describing these planning activities using the military metaphor of “military sand table planning” and “early deployment.”
3) Inability to rapidly add new topics: The pandemic also revealed the need for medical educators to engage in some topics traditionally not articulated in medical curricula. It was challenging to add new topics in the ongoing 2020 spring semester curricula but respondents suggested to add the following topics in the future: infectious disease control, emergent infectious disease, crisis management and communication, public policy and ethical issues related to pandemics such as distribution of medical resources, and government control and restrictions on human rights vs quarantine policy.
E. Opportunities
Taiwanese medical school deans highlighted three opportunities which enabled them to continue to open medical schools during the COVID-19 pandemic: centralised anti-epidemic policies, collaborations among medical schools, and educational innovations.
1) Centralised anti-epidemic policies: Taiwanese deans all reported that the policies from the central government are helpful in their implementation of anti-epidemic measures. Several deans shared the policy guidelines issued by the Ministry of Education with clear guidelines to follow the principles of infection containment. Although each university has the flexibility to decide how to comply with the guidelines, there was external oversight to ensure compliance. For example, when a teaching hospital had an intra-hospital transmission of COVID-19, the medical school had to work with the Central Epidemic Command Center and Ministry of Education in its response.
2) Inter-institutional collaborations: Collaborations among medical schools through the Taiwan Association of Medical Education (TAME) also helped Taiwanese medical school deans to adapt to COVID-19. For instance, the deans worked together at TAME to ensure that final-year students graduated on time. Every year, TAME organises a national OSCE examination required for graduation for final year Taiwanese medical students. Medical schools and teaching hospitals collaborated to administer these exams at OSCE centers in selected teaching hospitals with infection mitigating measures.
3) Educational innovations: All respondents mentioned that the COVID-19 pandemic provided opportunities to engage in innovations in medical education, especially online education. Online education was quickly implemented in some schools because access to internet is prevalent in Taiwan and they utilised the technology developed before the pandemic. One school reported an innovation using the Interactive Response System (IRS) developed three years ago and is now applied to enhance online teaching amid COVID-19. Another school adapted communication software instead of face-to-face counseling meetings. One school reported using “LINE” (a messaging app widely used in Taiwan) for a group chat for students to reduce student anxiety related to COVID-19.
F. Threats
Three themes were identified during the COVID-19 pandemic as threats to medical education, but external to medical schools: parental pressure to remove students from clinical settings, decrease in patient volume, and hospital infection control measures limited educational opportunities.
1) Parental pressure to remove students from clinical settings: Several deans mentioned that students’ parents reached out to them, pressuring them to discontinue clinical rotations. One respondent stated, “Parents are more worried than teachers and students. They are concerned that clinical rotations in the hospitals are risky for students. However, parents accepted our explanation that clinical rotations will not proceed unless there is adequate PPE and infection control measures.”
2) Decrease in patient volume: Another threat commonly mentioned was the decrease in patient volume. A participant explained, “Our hospital experienced a 30% decrease in patient volume. It is inconvenient for patients to come to the hospital due to tightened entrance control. The restriction on patients’ family visits is another factor. We are not letting students rotate on wards with suspected COVID-19 patients.” The limited patient encounters are perceived as potential threat to students’ clinical competence.
3) Hospital infection control measures limited educational opportunities: Finally, another threat reported was associated with infection control measures by the teaching hospitals. Deans expressed concerns that students’ clinical learning opportunities were compromised during the pandemic due to cancelled bedside teaching in high-risk specialties, cancelled presentations in conferences, cancelled interdepartmental grand rounds, and suspension of exchange programs both domestically and internationally. Some mentioned that reduced clinical exposures might result in less role modeling.
IV. DISCUSSION
During this historical event, medical schools around the world are challenged to navigate a path forward to meet missions of education, research, and patient care during an ongoing pandemic. As many countries are loosening or tightening restrictions after their curves of infection have flattened or resurged, medical schools globally are at various stages of deliberating when and how to resume campus-based and hospital-based medical education (Blaaza et al., 2020; Cleland et al., 2020; Tolsgaard et al., 2020). A systematic rapid review of published reports of medical educational developments in response to the COVID-19 pandemic concluded that most papers lacked evaluation data and focused on transitioning online and removing students from the clinical contexts (Gordon et al., 2020). The review suggested that medical schools learn from a few postgraduate papers reporting how face-to-face patient contact could be maintained while mitigating risk using PPE and social distancing (G. Choi et al., 2020; Hanel et al., 2020; Kang et al., 2020). Our study of medical school deans in Taiwan on how they continued in-person medical education throughout the COVID-19 pandemic offers lessons for the medical education community to engage medical students in campus-based and workplace-based learning with evaluation of impacts.
This study offers a conceptual advance by demonstrating how SWOT analysis can help us reflect on medical education adaptations to COVID-19 pandemic and future crises. Our analysis of the strengths, weaknesses, opportunities and threats in Taiwanese medical school adaptations to COVID-19 highlights certain strategies to leverage strengths and opportunities to overcome weaknesses and threats. A critical factor in the decision to continue face-to-face medical education, clearly identified by the opportunity-strength strategy in Table 3, was the early deployment of epidemic prevention measures under centralised government policies and strong medical school leadership. Epidemic prevention measures were deployed at all levels of schools in Taiwan as students returned to campus for spring semester in February 2020. To enact anti-epidemic policies in different contexts, this study presented various preventive measures to keep the recommended social distance in classrooms, laboratories, and teaching hospitals. To implement these measures, transparent communication and administrative support from medical school leadership are essential.
SWOT analysis on opportunity-weakness and threat-weakness strategies offers lessons on how to overcome the weakness of lack of faculty confidence in online education. Although online education is an important curricular adaptation to maintain social distance in campus-based medical education, our survey shows that respondents found online teaching challenging to faculty and are concerned about the effectiveness of online education. Strategies identified to overcome this weakness is to take advantage of the educational technology readily available and to transform the threats from hospital infection control to suspend hospital-based education into opportunities for integrating innovative online education. It is important to leverage innovative online education in workplace learning in the context of reduced patient case exposures before the pandemic subsides (B. Choi et al., 2020; Lo et al., 2020). There is sufficient evidence in the education literature that well-designed online education is as effective as traditional classroom teaching and shows equivalent or better learning outcomes (George et al., 2014; Jung & Rha, 2000; Khalil et al., 2020). We hope that the evaluations reported in the fall semester survey showing equivalent outcomes of online adaptations during COVID-19 would encourage medical educators to take advantage of innovations reported by this study, existing literature on online education in general, and the growing literature about innovative online medical education (Ahmed et al., 2020; Medical Education, 2020).
This study highlighted that another enabling factor for Taiwanese medical educators to continue face-to-face medical education was the experience of SARS. The Taiwanese population became accustomed to anti-epidemic measures, including wearing masks after SARS, which facilitated the implementation of anti-epidemic measures in schools during COVID-19. Taiwanese health providers were severely challenged during the 2003 SARS epidemic. 103 of 318 confirmed cases (Centers for Disease Control and Prevention, 2003) and 11 of 60 deaths (including two first-year residents) (Taiwan Centers for Disease Control, 2013) were healthcare workers. Medical education leaders had a difficult decision to make regarding the final year students who were working as interns in hospitals (Lai, 2020). Following closures of clinics and resignation of healthcare providers, there were heated debates about physician duties to treat patients while being at risk of exposure to a deadly infectious disease and of being stigmatised by society (Lee, 2003). After SARS, not only were curricula on ethics and infection control strengthened, but the medical education system was reformed to convert the final-year of medical school to a formal post-graduate year program (Ho et al., 2017). In addition, as articulated by the respondents of the survey, SARS prepared Taiwanese medical educators and clinical teachers to be confident and competent to perform their educational and clinical duties in the time of COVID-19.
Although this study has many lessons to offer both conceptually and practically, there are some limitations to be considered. We conducted the survey with open-ended questions to explore diverse perspectives. The reported theme frequencies should be considered with caution since some respondents record more comprehensive answers than others. While the most frequently mentioned themes might be most important to the respondents, the least frequently given answer might be valuable due to its innovative nature. Another limitation of an open-ended questionnaire is that respondents might not have the time to enter answers in detail. To overcome this limitation, we invited the respondents to participate in a follow-up interview. However, only about one-third of deans were available to be interviewed during the study period. The four interviews conducted nonetheless enriched the study with more context and details. Finally, this study only surveyed medical school deans. It would be interesting to conduct further studies comparing these results to the perspectives of students and faculty members.
V. CONCLUSION
This nationwide study of all medical schools in Taiwan documents critical observations of top medical school leaders during an active pandemic. This case study demonstrated that strengths and opportunities such as strong leadership and centralised anti-epidemic policies can overcome weaknesses and threats such as faculty lack of confidence in online education and parental pressure to stop hospital-based education. We recommend that medical school leaders conduct SWOT analyses as early as possible to plan strategies to continue safe and quality medical education during COVID-19 and forthcoming emergencies. Similar to the impact of SARS, which led to reform of the Taiwanese postgraduate training system, there is hope that thoughtful reflection on medical education adaptations to the COVID-19 pandemic will improve medical education in general and lead to better preparation for future crises.
Notes on Contributors
MH contributed to the conception, acquisition and analysis of data, drafted the article, and approved the final version; YC contributed to the design, acquisition and analysis of data, drafted the article, and approved the final version; SK contributed to analysis and interpretation of data, revised the article critically, and approved the final version.
Ethical Approval
This study was approved as exempt by the Georgetown University Institutional Review Board (STUDY00002812). Since the study poses no greater than minimal risk to subjects, a waiver of written consent was granted. . We emailed invitations with information about study purpose, data confidentiality, and a weblink to the online survey. A verbal consent was obtained before data collection began. Participation was voluntary without incentives offered. All methods were carried out in accordance with relevant guidelines and regulations.
Data Availability
It is not possible to share data since we did not get consent from participants to share all data collected. They agreed to have results reported in a summary format with selected quotes.
Acknowledgement
The authors wish to thank survey respondents and interviewees for providing insights on the research topic. Fred Hafferty and Carrie Chen provided useful feedback to improve the manuscript.
Funding
This study did not receive any funding.
Declaration of Interest
The authors declare that they have no competing interests.
References
Abbas, M., Dhane, M., Beniey, M., Meloche-Dumas, L., Eissa, M., Guerard-Poirier, N., El-Raheb, M., Lebel-Guay, F., Dubrowski, A., & Patocskai, E. (2020). Repercussions of the COVID-19 pandemic on the well-being and training of medical clerks: A pan-Canadian survey. BMC Medical Education, 20(1), 385. https://doi.org/10.1186/s12909-020-02293-0
Ahmed, S. A., Hegazy, N. N., Abdel Malak, H. W., Cliff Kayser, W., 3rd, Elrafie, N. M., Hassanien, M., Al-Hayani, A. A., El Saadany, S. A., Ai-Youbi, A. O., & Shehata, M. H. (2020). Model for utilizing distance learning post COVID-19 using (PACT)TM a cross sectional qualitative study. BMC Medical Education, 20(1), 400. https://doi.org/10.1186/s12909-020-02311-1
Al-Balas, M., Al-Balas, H. I., Jaber, H. M., Obeidat, K., Al-Balas, H., Aborajooh, E. A., Al-Taher, R., & Al-Balas, B. (2020). Distance learning in clinical medical education amid COVID-19 pandemic in Jordan: Current situation, challenges, and perspectives. BMC Medical Education, 20(1), 341. https://doi.org/10.1186/s12909-020-02257-4
Association for Medical Education in Europe. (2020). COVID-19. Retrieved April 1, 2021, from https://amee.org/covid-19
Association of American Medical Colleges. (2021). Coronavirus (COVID-19) resource hub. Retrieved April 1, 2021, from https://www.aamc.org/coronavirus-covid-19-resource-hub
Blaaza, M., Akhtar, H. N., & Tanzim, U. (2020). Returning to clinics amidst COVID-19: A student response to Compton et al. Medical Education, 54(12), 1193. https://doi.org/10.1111/medu.14282
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative research in psychology, 3(2), 77-101.
Centers for Disease Control and Prevention. (2003). Severe acute respiratory syndrome–Taiwan, 2003. Morbidity and mortality weekly report, 52(20), 461‐466.
Chang Gung University. (2020, March 16). Chang Gung University COVID-19 anti-epidemic advanced adaptation measures [Video]. YouTube. https://www.youtube.com/watch?v=WyoOoShXVa8
Choi, B., Jegatheeswaran, L., Minocha, A., Alhilani, M., Nakhoul, M., & Mutengesa, E. (2020). The impact of the COVID-19 pandemic on final year medical students in the United Kingdom: a national survey. BMC medical education, 20(1), 206. https://doi.org/10.1186/s12909-020-02117-1
Choi, G., Wan, W., Chan, A., Tong, S., Poon, S., & Joynt, G. (2020). Preparedness for COVID-19: In situ simulation to enhance infection control systems in the intensive care unit. British Journal of Anaesthesia, 125(2), e236-e239. https://doi.org/10.1016/j.bja.2020.04.001
Cleland, J., McKimm, J., Fuller, R., Taylor, D., Janczukowicz, J., & Gibbs, T. (2020). Adapting to the impact of COVID-19: Sharing stories, sharing practice. Medical Teacher, 42(7), 772-775. https://doi.org/10.1080/0142159X.2020.1757635
Compton, S., Sarraf-Yazdi, S., Rustandy, F., & Radha Krishna, L. K. (2020). Medical students’ preference for returning to the clinical setting during the COVID-19 pandemic. Medical Education, 54(10), 943-950. https://doi.org/10.1111/medu.14268
Frieden, J. (2020, May 9). Medical schools grapple with challenges for the coming year— Three-quarters hope to have students back by the end of July. MedPage Today. Retrieved April 1 fromhttps://www.medpagetoday.com/publichealthpolicy/medicaleducation/86416
Fu Jen Catholic University. (2020, February 16). COVID-19: Fu Jen Catholic University anti-epidemic promotion video. [Video]. YouTube. https://youtu.be/-n3KvlVHpzY
Gardner, L. (2020, January 31). Update January 31: Modeling the spreading risk of 2019-nCoV. Johns Hopkins University Center for Systems Science and Engineering. Retrieved April 1 from https://systems.jhu.edu/research/public-health/ncov-model-2/
George, P. P., Papachristou, N., Belisario, J. M., Wang, W., Wark, P. A., Cotic, Z., Rasmussen, K., Sluiter, R., Riboli-Sasco, E., Tudor Car, L., Musulanov, E. M., Molina, J. A., Heng, B. H., Zhang, Y., Wheeler, E. L., Al Shorbaji, N., Majeed, A., & Car, J. (2014). Online eLearning for undergraduates in health professions: A systematic review of the impact on knowledge, skills, attitudes and satisfaction. Journal of Global Health, 4(1), 010406. https://doi.org/10.7189/jogh.04.010406
Ghazinoorya, S., Abdia, M., & Azadegan-Mehr, M. (2011). SWOT methodology: A state-of-the-art review for the past, a framework for the future. Journal of Business Economics and Management, 12(1), 24-48. https://doi.org/10.3846/16111699.2011.555358
Gordon, L., & Cleland, J. A. (2021). Change is never easy: How management theories can help operationalise change in medical education. Medical Education, 55(1), 55-64. https://doi.org/10.1111/medu.14297
Gordon, M., Patricio, M., Horne, L., Muston, A., Alston, S. R., Pammi, M., Thammasitboon, S., Park, S., Pawlikowska, T., Rees, E. L., Doyle, A. J., & Daniel, M. (2020). Developments in medical education in response to the COVID-19 pandemic: A rapid BEME systematic review: BEME Guide No. 63. Medical Teacher, 42(11), 1202-1215. https://doi.org/10.1080/0142159X.2020.1807484
Hanel, E., Bilic, M., Hassall, K., Hastings, M., Jazuli, F., Ha, M., Trotter, B., Fraser, C., & Rutledge, G. (2020). Virtual application of in situ simulation during a pandemic. Canadian Journal of Eemergency Medicine, 22(5), 563-566. https://doi.org/10.1017/cem.2020.375
Harries, A. J., Lee, C., Jones, L., Rodriguez, R. M., Davis, J. A., Boysen-Osborn, M., Kashima, K. J., Krane, N. K., Rae, G., Kman, N., Langsfeld, J. M., & Juarez, M. (2021). Effects of the COVID-19 pandemic on medical students: A multicenter quantitative study. BMC Medical Education, 21(1), 14. https://doi.org/10.1186/s12909-020-02462-1
Ho, M.-J., Shaw, K., Shih, J., & Chiu, Y.-T. (2017). Mission and modernity: The history and development of medical education in Taiwan. In L. C. Chen, M. R. Reich, & J. Ryan (Eds.), Medical Education in East Asia: Past and Future (pp. 84-111). Indiana University press.
International Association of Medical Science Educators. (2020, April 22). #IAMSECafe Archives & COVID-19 resources for medical science educators. Retrieved April 1 from http://www.iamse.org/covid-19-resources-for-medical-science-educators/
Journal of the Association of American Medical Colleges. (2021). COVID-19 and medical education. Retrieved April 1 from https://journals.lww.com/academicmedicine/pages/collectiondetails.aspx?TopicalCollectionId=68
Jung, I., & Rha, I. (2000). Effectiveness and cost-effectiveness of online education: A review of the literature. Educational Technology, 40(4), 57-60.
Kang, Y., Deng, L., Zhang, D., Wang, Y., Wang, G., Mei, L., Zhou, G., & Shu, H. (2020). A practice of anesthesia scenario design for emergency cesarean section in patients with COVID-19 infection based on the role of standard patient. BioScience Trends, 14(3), 222-226. https://doi.org/10.5582/bst.2020.03066
Keegan, D. A., & Bannister, S. L. (2021). More than moving online: Implications of the COVID-19 pandemic on curriculum development. Medical Education, 55(1), 101-103. https://doi.org/10.1111/medu.14389
Khalil, R., Mansour, A. E., Fadda, W. A., Almisnid, K., Aldamegh, M., Al-Nafeesah, A., Alkhalifah, A., & Al-Wutayd, O. (2020). The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: A qualitative study exploring medical students’ perspectives. BMC Medical Education, 20(1), 285. https://doi.org/10.1186/s12909-020-02208-z
Lai, C. (2020, March 20). 2003 SARS: Reflections on Taiwanese medical education. UDN. https://health.udn.com/health/story/6631/4421448
Lazarus, G., Findyartini, A., Putera, A. M., Gamalliel, N., Nugraha, D., Adli, I., Phowira, J., Azzahra, L., Ariffandi, B., & Widyahening, I. S. (2021). Willingness to volunteer and readiness to practice of undergraduate medical students during the COVID-19 pandemic: A cross-sectional survey in Indonesia. BMC Medical Education, 21(1), 138. https://doi.org/10.1186/s12909-021-02576-0
Lee, M. (2003). SARS 風暴的啟示[Learning from the SARS event] [Editorial]. Journal of Medical Education, 7(1), 1-2.
Lo, H.-Y., Lin, S.-C., Chaou, C.-H., Chang, Y.-C., Ng, C.-J., & Chen, S.-Y. (2020). What is the impact of the COVID-19 pandemic on emergency medicine residency training: An observational study. BMC Medical Education, 20(1), 348. https://doi.org/10.1186/s12909-020-02267-2
Medical Education. (2020, May 7). Medical education adaptations. Retrieved April 1, 2020, from https://onlinelibrary.wiley.com/doi/toc/10.1002/(ISSN)1365-2923.med.adaptations.vi
Reid, M. D., & Sam, A. H. (2021). Reflections on assessment in the wake of change from the COVID-19 pandemic. Medical Education, 55(1), 128-130. https://doi.org/10.1111/medu.14368
Soled, D., Goel, S., Barry, D., Erfani, P., Joseph, N., Kochis, M., Uppal, N., Velasquez, D., Vora, K., & Scott, K. W. (2020). Medical student mobilization during a crisis: Lessons from a COVID-19 medical student response team. Academic Medicine, 95(9), 1384-1387. https://doi.org/10.1097/ACM.0000000000003401
Taiwan Center for Disease Control. (2020). Prevention and control of COVID-19 in Taiwan. Retrieved April 1, 2021, from https://www.cdc.gov.tw/Category/Page/0vq8rsAob_9HCi5GQ5jH1Q
Taiwan Centers for Disease Control. (2013). Severe acute respiratory syndrome (SARS). Retrieved April 1, 2021 from https://www.cdc.gov.tw/File/Get/InG8jagjxffXBDW1UexnrA
Tolsgaard, M. G., Cleland, J., Wilkinson, T., & Ellaway, R. H. (2020). How we make choices and sacrifices in medical education during the COVID-19 pandemic. Medical Teacher, 42(7), 741-743. https://doi.org/10.1080/0142159X.2020.1767769
Topor, D. R., Dickey, C., Stonestreet, L., Wendt, J., Woolley, A., & Budson, A. (2018). Interprofessional health care education at academic medical centers: Using a SWOT analysis to develop and implement programming. MedEdPORTAL, 14, 10766. https://doi.org/10.15766/mep_2374-8265.10766
UNICEF. (2021). COVID-19 Education: From disruption to recovery. Retrieved April 1, 2021, from https://en.unesco.org/covid19/educationresponse
Wang, C. J., Ng, C. Y., & Brook, R. H. (2020). Response to COVID-19 in Taiwan: Big data analytics, new technology, and proactive testing. The Journal of the American Medical Association, 323(14), 1341-1342. https://doi.org/10.1001/jama.2020.3151
Zhu, N., Zhang, D., Wang, W., Li, X., Yang, B., Song, J., Zhao, X., Huang, B., Shi, W., Lu, R., Niu, P., Zhan, F., Ma, X., Wang, D., Xu, W., Wu, G., Gao, G. F., & Tan, W. (2020). A novel coronavirus from patients with pneumonia in China, 2019. The New England Journal of Medicine, 382(8), 727-733. https://doi.org/10.1056/NEJMoa2001017
*Yu-Che Chang
No. 5, Fuxing St.,
Guishan Dist.,
Taoyuan City 333012,
Taiwan (R.O.C.)
Tel: +886-33281200 ext 3807
Email: changyuche@gmail.com
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









