Enhancing the student experience through sustainable Communities of Practice
Submitted: 29 March 2021
Accepted: 28 September 2021
Published online: 4 January, TAPS 2022, 7(1), 102-105
https://doi.org/10.29060/TAPS.2022-7-1/SC2508
Mairi Scott & Susie Schofield
Centre for Medical Education (CME), School of Medicine, University of Dundee, Scotland, United Kingdom
Abstract
Introduction: The switch to online off-campus teaching for universities worldwide due to COVID-19 will transform into more sustainable and predictable delivery models where virtual and local student contact will continue to be combined. Institutions must do more to replace the full student experience and benefits of learners and educators being together.
Methods: Our centre has been delivering distance blended and online learning for more than 40 years and has over 4000 alumni across five continents. Our students and alumni come from varied healthcare disciplines and are at different stages of their career as educators and practitioners. Whilst studying on the programme students work together flexibly in randomly arranged peer groups designed to allow the establishment of Communities of Practice (CoP) through the use of online Discussion Boards.
Results: We found Discussion Boards encouraged reflection on learning, sharing of ideas with peers and tutors, reduce anxiety, support progression, and enable benchmarking. This led to a highly effective student sense of belonging to each other, our educators, and the wider University, with many highlighting an excellent student experience and maintaining a thriving CoP within the alumni body.
Conclusion: Despite being based on one large postgraduate programme in medical education, our CoP approach is relevant to any undergraduate programme, particularly those that lead to professional qualification. With our mix of nationalities, we can ‘model the way’ for enabling strong CoP’s to share ideas about best practice with a strong student and alumni network which can be shared across the international healthcare community.
Keywords: Communities of Practice, Sense of Belonging, Student Experience
I. INTRODUCTION
The sudden switch to online, dual delivery and on-campus/off-campus teaching for Universities worldwide will not be reversed at the end of the current COVID-19 crisis but will transform into a more sustainable and predictable delivery model where virtual and local student contact will continue to be combined. The switch, known as Emergency Remote Teaching (ERT) (Hodges et al., 2020) achieved much in a short timeframe but institutions need to do more to truly replace the full student experience and benefits of learners and educators being together on-site. The need for this new approach is acute in professional-based courses such as medicine where students need to learn complex skills within the context of healthcare delivery. These skills are acquired through multiple interactions with clinical colleagues in the workplace which, although often brief, are focused in real-time.
Given that the learning environment is dependent on the institutional ‘personality, spirit, and culture’ (Holt & Roff, 2004, pp. 553), human interaction is necessary to create that culture. We must develop new approaches to delivering medical education by merging established educational technologies with virtual approaches to establish on-line interaction with peers and senior colleagues such as can be achieved in Communities of Practice (CoPs) (Lave & Wenger, 1991). CoPs are social structures where people can share ideas, stories, and experiences relevant to the community’s activities. They help participants make sense of new knowledge and enable novices to benefit from working with experts, thus reducing anxiety, supporting progression, and enabling benchmarking. These components lead to the creation of a rich environment for information-sharing which has become increasingly important within healthcare delivery organisations during the COVID-19 pandemic.
We have built on over 40 years’ experience of delivering distance, blended and online Masters-level accredited medical education learning across five continents to ‘model the way’ to providing a strong student experience for online learners. Our students and alumni come from various interdisciplinary healthcare disciplines, at different stages of their career as educators and practitioners.
II. METHODS
Several Discussion Boards (DBs), usually one per study week plus one for assignment questions are created in each 12-week Moodle-based module. Students are randomly assigned to groups to work together flexibly within these peer groups. Each discussion has a ‘prompt’ linked to that week’s work, designed to create CoPs and a highly effective student sense of belonging (SoB) to each other and programme educators. In the first module students are actively encouraged to participate, with emphasis being on the ‘safe space’ created that allows them to learn effectively from and with each other. DB comments are used as part of programme enhancement and quality assurance. Students give informed consent to their evaluation comments within DBs being extracted for overall programme review.
III. RESULTS
As students move from legitimate peripheral participant to experienced member, they often express increased confidence that their posts will allow them to share their view and help colleagues. The forum posts have been analysed as part of a much larger study; the following diagram (Figure 1) highlights some of the benefits.
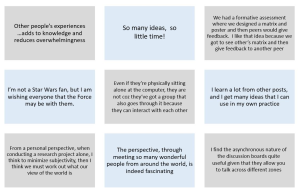
Figure 1. Sample of comments in DBs posts
Our experience over the last four years is that student levels of interaction increase the further into the programme they go, suggesting that they value and enjoy it. Overall, when asked specifically if that assumption is correct, feedback from students is exceptionally positive and they comment on their achievement of a SoB through engagement with the DBs. Many highlight the excellent student experience. Another indirect indication of success is that student module success rate averages 93% across the modules, which is high for an online learning programme.
The benefits of using DBs are threefold:
- They allow for reflection on learning in real-time due to regular module-specific weekly activities requiring students to reflect on that week’s educational materials and post their thoughts on the DBs.
- They allow sharing with peers and tutors, establishing CoPs: The DB posts create peer-to-peer dialogue, encouraging students to practise the language of the discipline in a safe, supported environment. Learning activities are based on the principle of linking previous experience with the interpretation of new knowledge, thus enabling an escalation of the complexity of questions to enhance deeper connection and dialogue. Although essentially (and importantly) it is the students as peers who are encouraged to respond to each other’s questions and comments, the tutors do monitor posts, providing input when necessary and desirable. In some modules, students are required to give peer feedback on draft assignments using a 1:4 ratio to encourage a range of views and expertise, increasing the depth and extent of their critical thinking and analysis. This also gives them practice in giving and receiving feedback, an essential skill for future medical educators.
- CoPs build trust in colleagues and a SoB within the learning environment, leading to an excellent learning experience. Students state that they value the tutor contribution as this increases the confidence they have in their own online comments, sometimes shifting the discussion to a more profitable area for new learning in a way that was not pre-planned or even at times expected.
IV. DISCUSSION
Our approach to the creation of CoPs is based on the principle that in order to establish student trust and a SoB DBs are an essential tool. Management research describes trust within organisations as being multifaceted, with the main components being capability, well-meaning intent, and integrity (Ridings et al., 2002). It is accepted that within our programmes both tutor and student capabilities have been established. Integrity is established by clearly explaining the expected mode of student behaviour at the outset and demonstrated as students work through the programme. Well-meaning intent is demonstrated by acts of positive reciprocation built up over time by asking students to give peer feedback frequently and around increasingly complex activities. Both integrity and well-meaning intent therefore need to have a continued focus during module design and delivery and throughout the assessment process.
Now that medical education has been forced to re-evaluate the place of online learning as a consequence of the COVID-19 crisis, it seems inevitable that many of the discovered benefits will lead to significant changes in the way we teach and learn. Davis (2018) explored a future medical school being one ‘without walls’ by which he meant that the artificial separation of the ‘classroom and the clinic’ would inevitably diminish as we embraced flipped classrooms and online collaborative learning.
If we adopt this approach for student learning it may also change the way we think about faculty development, as we could create extensive networks of faculty development special interest grouped CoPs beyond the ‘walls’ of our own schools. A recent study by Chan et al. (2018) in McMaster describes the creation of a Faculty Incubator – a virtual CoP which uses a longitudinal, asynchronous, online platform to deliver a one-year curriculum to support early-to mid-career educators from 30 different locations with their professional development. This widespread (geographically) collaborative approach was found to be well received, with lively interactions which broke down some of the boundaries that normally prevent early career academics from approaching unknown colleagues in different locations, colleagues they would normally never have met in person.
An additional challenge created by the COVID-19 pandemic was the necessity for healthcare professionals to make clinical decisions in an ‘evidence-poor’ disease by gathering emerging data (often by word-of-mouth) and treating patients without the certainty of a knowledge base built up over decades of robust randomised controlled trial (RCT) evidence. This is described by Rosenquist (2021, pp. 8) as a kind of “Bayesian fatigue”: a stress-induced dysphoria experienced when the corpus of knowledge that is the foundation of one’s work acquired over decades, becomes less important than information being gathered from disparate sources in real time.’ The ‘disparate sources’ referred to here are groups of widely dispersed practitioners (within current and new CoPs) who are sharing individual and collective rapid learning by experience that has become necessary when treating patients with COVID-19. These CoPs are based on the collective trust healthcare professionals express in valuing the views of colleagues struggling with similar challenges. This helps reduce that ‘Bayesian’ impact when it comes to making difficult clinical decisions in real time with limited evidence. However, trust within a CoP also comes from previous positive experience of being within other CoPs, and so it is important that we as medical educators enable our students to have experience of the value of sustainable CoPs in their own learning. Despite the limitations of the range of the study comments, we believe that given the extent of the sudden switch to ERT our findings of use of DBs to establish much appreciated CoPs justifies early dissemination through this short communication.
V. CONCLUSION
As medical educators we must have the skills necessary to establish strong and sustainable CoPs to educate current and future healthcare professionals in this effective way of learning from each other. This can be done as effectively with online learning as with on-campus interaction, allowing the possibility of the widespread creation of truly effective international CoPs sustainable for years to come.
Notes on Contributors
Professor Mairi Scott reviewed the literature, selected the data, wrote the manuscript, created the presentation and presented the materials virtually to the Conference. Dr Susie Schofield reviewed the literature, advised on the selection of the data and gave critical feedback on the manuscript. Both authors have read and approved the final manuscript.
Ethical Approval
Ethics approved was granted by School of Medicine & School of Life Sciences Research Ethics Committee, University of Dundee, Dundee, DD1 4HN on 03/05/19. Application Number: 19/41.
Data Availability
Ethical approval specified that raw data would not be made available for others out with the Centre ‘beyond the anonymised published or reported versions within the dissemination strategy’.
Acknowledgement
The authors would like to thank Dr Thillainathan Sathaananthan (PhD student) and Dr Linda Jones (PhD supervisor, Senior Lecturer) CME, University of Dundee, who produced some of the outcomes as part of research into student experiences with online learning and the use of Discussion Boards.
Funding
No grant or external funding was received for this work.
Declaration of Interest
Both authors have no conflict of interest to declare.
References
Chan, T. M., Gottlieb, M., Sherbino, J., Cooney, R., Boysen-Osborn, M., Swaminathan, A., Ankel, F., & Yarris, L. M. (2018). The ALiEM faculty incubator: A novel online approach to faculty development in education scholarship. Academic Medicine, 93(10), 1497–1502. https://doi.org/10.1097/ACM.0000000000002309
Davis, D. (2018). The medical school without walls: Reflections on the future of medical education. Medical Teacher, 40(10), 1004–1009. https://doi.org/10.1080/0142159X.2018.1507263
Hodges, C., Moore, S., Lockee, B., Trust, T., & Bond, A. (2020). The difference between emergency remote teaching and online learning. EDUCAUSE Review. https://er.educause.edu/%20articles/2020/3/the-difference-between-emergency-remote-teaching-and-online-learning
Holt, M. C., & Roff, S. (2004). Development and validation of the Anaesthetic Theatre Educational Environment Measure (ATEEM). Medical Teacher, 26(6), 553-558. https://doi.org/10.1080/01421590410001711599
Lave, J., & Wenger, E. (1991). Situated learning: Legitimate peripheral participation. Cambridge University Press.
Ridings, C. M., Gefen, D., & Arinze, B. (2002). Some antecedents and effects of trust in virtual communities: The Journal of Strategic Information Systems, 11(3-4), 271–295. https://doi.org/10.1016/S0963-8687(02)00021-5
Rosenquist, J. N. (2021). The stress of Bayesian medicine—Uncomfortable uncertainty in the face of COVID-19. New England Journal of Medicine, 384(1), 7-9. https://doi.org/10.1056/NEJMp2018857
*Mairi Scott
Centre for Medical Education,
University of Dundee
Email: m.z.scott@dundee.ac.uk
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









