Biomedical students’ course preference and links with quality of life and psychological distress
Submitted: 23 January 2021
Accepted: 11 August 2021
Published online: 4 January, TAPS 2022, 7(1), 55-65
https://doi.org/10.29060/TAPS.2022-7-1/OA2475
Marcus A Henning1, Vanamali Joseph1, Roger J Booth2, Christian U Krägeloh3 & Craig S Webster1
1School of Medicine, University of Auckland, New Zealand; 2Department of Medical Science, University of Auckland, New Zealand; 3Department of Psychology and Neuroscience, Auckland University of Technology, New Zealand
Abstract
Introduction: This study investigates psychological distress and quality of life (QoL) amongst first year premedical and health science students. The primary aim of this study was to investigate potential differences in QoL and psychological distress between students who sought entry into a medicine programme when compared to those opting for a non-medicine career.
Methods: We examined participant responses to measures of QoL, psychological distress, and course preference (medicine or other). A structural equation model was conducted to consider the interrelationships among future course preference, gender, QoL, depression, anxiety and stress.
Results: Three hundred and sixty-five students completed the online survey. An a priori conceptual model was developed and then evaluated using a structural equation model. The values obtained for RMSEA (0.027), CFI (0.999), and SRMR (0.016) indicated an excellent model fit. The overall model fit statistic, chi-square (χ2 = 7.626, df=6, p= .267), confirmed a good model fit. Students aiming to enrol in medicine generated higher psychological health and environmental QoL scores compared to their non-medicine oriented peers. In addition, physical QoL and psychological health QoL scores significantly predicted psychological distress measures.
Conclusion: The study raises a potential debate regarding placing students with mixed career intentions into the same course and the potential implications this may have on teaching in interprofessional and large student groups in relation to wellbeing, pedagogy, equity, and expenditure. The findings clearly indicated that medical students are not as adversely impacted upon in terms of QoL and psychological distress compared with their non-medical peers.
Keywords: Medical and Health Science Students, Quality of Life, Psychological Distress, Course Preference
Practice Highlights
- Students focusing on medicine report higher levels of psychological health and environmental QoL.
- Course preference is associated with psychological QoL and psychological distress.
- Issues with psychological QoL are more common among females.
- QoL and learning in large lecture theatres requires further investigation.
I. INTRODUCTION
At the University of Auckland, the Biomedical Common Year or Overlapping Year 1 (BCY) programme is a first-year syllabus and the gateway for many students aiming to enrol into either medicine or other healthcare disciplines (e.g., nursing, optometry, or pharmacy). The requirements for entry into medicine is highly competitive such that approximately 700 students who study in BCY aim to apply for medicine out of which only 250 students are chosen (Henning et al., 2017b). Entry into other healthcare disciplines (e.g., nursing, optometry, or pharmacy) is less competitive and selection is thus likely less distressing (Al Alwan et al., 2013). However, the large class sizes within the pre-medical and health science year (of approximately 1,300 students) containing students applying for either medicine or non-medicine programmes may also create a marginalising learning dynamic that may hinder the motivation and wellbeing of non-medicine students (Henning et al., 2017a). Hence, the aim of this research was to assess whether those students aiming for selection into medicine were more at risk of poor quality of life (QoL) and psychological distress relative to those students aiming for selection into other healthcare disciplines.
Numerous studies have researched the areas of QoL and psychological distress amongst medical students (Lovibond & Lovibond, 1995; Szabó, 2010; Wickramasinghe et al., 2019). In their systematic review, Dyrbye et al. (2006) reported concerning rates of depression, anxiety and general psychological distress among medical students, citing for example in one report that 37% of medical students in their first year of study experienced mental health issues of some kind. The adverse impact of distress among students can contribute to problems associated with academic attainment, professional development, academic honesty, substance abuse, cynicism, humanitarian attitude, and development of empathy. Moreover, psychological distress appears to be more of a concern among female medical students. The implication underlying the research investigating QoL and psychological distress suggests that medical students are more compromised than their non-medical peers.
Our conceptual model for the present study was developed in accordance with self-determination theory (Ryan & Deci, 2000). According to this theory, the act of choosing can positively affect motivation, well-being and learning if the needs for autonomy, relatedness, and competence in the individual are high. In this study, students were free to choose their course of study and hence freedom of choice was perceived as equivalent to the notion of course preference. According to this theory, students can be intrinsically motivated (engaged in their studies because of inherent enjoyment) and extrinsically motivated with a focus on outcome (Vansteenkiste et al., 2006). Extrinsic motivation, however, can be differentiated into aspects of regulation dependent upon the degree of autonomy. Therefore, there are facets of autonomous motivation (which involves volition and choice) versus that of controlled motivation (feeling pressured or coerced) (Vansteenkiste et al., 2006). Hence, intrinsic motivation and well-intentioned aspects of extrinsic motivation are considered autonomous, whilst the poorly internalised form of extrinsic motivation are less well incorporated into an individual’s sense of self. In our proposed model, we suggest features of choice with links to QoL.
We cannot assume that the medical or non-medical students differ in terms of their intrinsic or extrinsic motivation, but we do know that the majority of non-medical students at this university (e.g. nursing and pharmacy) have been given conditional entry into their courses on the proviso that they pass their courses in the BCY. However, medical students do not have this luxury and are in a more competitive mode of action. They are, thus, likely intrinsically and extrinsically motivated, and their extrinsic motivation could be either autonomous or controlled. Our assumption is that the non-medical students are also likely to be intrinsic and extrinsically motivated, but their extrinsic motivation is likely more autonomous as they have conditional entry. Therefore, non-medical students would likely experience more heightened levels of QoL than medical students who are experiencing higher levels of competition (Katz & Assor, 2007; Ryan & Deci, 2000). If this is not true another more pressing variable may be affecting the QoL outcome, such as mixing high numbers of students together from different disciplines into one course (Hornsby & Osman, 2014). In addition, given the established empirical evidence (Haist et al., 2000; Henning et al., 2013; Naylor et al., 2018; Ramsbottom-Lucier et al., 1995), we argued that gender would likely moderate choice and QoL. Therefore, the first stage of our conceptual model proposes that, once students have chosen a particular course of study (medicine or other) this will directly impact their QoL given the increased expectation associated with the decision process (Katz & Assor, 2007). Therefore, those students aiming for a programme (i.e., medicine) requiring higher stakes will likely be more at risk of ill-health.
The next element of our argument proposes that QoL will likely impact psychological distress. For example, if a student experiences good health-related physical QoL they are then likely to have lowered risk of psychological distress (Burris et al., 2009). In their study of first year medical students, Verger et al. (2009) reported that psychological distress was moderated by gender and influenced by wellbeing protective factors, such as social support, coping with academic pressure, and socio-economic factors. Consequently, we suggest that there is likely a follow-on effect such that those students with compromised QoL will likely experience more psychological distress (Dyrbye et al., 2006). Nonetheless, the causes of poor QoL are likely complex and vary substantially between individuals given that some studies have shown that students aiming to study medicine may be more motivated and experience higher levels of QoL (Henning et al., 2017a).
The primary aim of this study was to empirically investigate potential differences in QoL and psychological distress between students who sought entry into a medicine programme when compared to those opting for a non-medicine career. The issue of follow-on effects from QoL to psychological distress has not been studied within this learning context. To illustrate potential differences between the two groups, we scrutinised conceptual links between choice, gender, QoL and psychological distress in reference to students’ course preference (medicine or other) whilst studying in the BCY programme.
II. METHODS
A. Participants
All students (N=1277) studying within the BCY programme were invited to participate in this survey. Students aiming to study in any health-related course at the University of Auckland first enrol in the BCY programme in preparation for formalised entry into degrees for Bachelor of Health Science, Bachelor of Pharmacy, Bachelor of Optometry or Bachelor of Medicine (The University of Auckland, 2019).
B. Procedure
Ethics approval for the collection and use of data was obtained from the University of Auckland Human Participants Ethics Committee (Ref. 021985).
Students were informed about the study by email in late July (2018), and two reminder emails were sent out. The anonymous survey was conducted prior to final course completion in Semester 2 (2018), but after grades for the first semester had been released. Informed consent was implied given that study participants received a participant information sheet prior to the start of the questionnaire. Data were collected online using a Google Forms questionnaire (Google.com, 2015), which requires respondents to fully complete the survey before they are able to submit it.
C. Measures
Demographic and background details were obtained to assess the representativeness of the sample included: (1) Age in years; (2) Gender; (3) Future course preference (medicine or other); (4) Enrolment status (international or domestic); and (5) Ethnicity.
Quality of life was measured using the New Zealand version of the WHOQOL (NZ WHOQOL-BREF) questionnaire (Krägeloh et al., 2016). It has four domains (physical QoL, psychological health QoL, social relationships QoL and the environmental QoL) and contains 31 items. In this study, physical QoL had six items, psychological health QoL had 10 items, social relationships QoL had four items and environmental QoL had eight items (The NZ WHOQOL Group, 2017). Questions 1 and 2 are global QoL and health items and, thus, not included in the scoring of the four quality of life domains. Question 3 was deemed to have little relevance with respect to the research question and had been previously identified as having a ceiling effect in early career medical students (Krägeloh et al., 2011). All items utilised a 5-point Likert scale with varying anchors (the scores for two items were reversed). High scores indicated higher levels of QoL.
Psychological distress was measured using the Depression, Anxiety and Stress Scale (DASS-21), which captures respondents’ emotional states in reference to three domains: depression, anxiety and stress (within the past seven days). Each domain is comprised of seven items. The DASS-21 instrument has been developed from a previous 42-item version (Lovibond & Lovibond, 1995), and has undergone psychometric investigation among a variety of populations (Le et al., 2017; Medvedev et al., 2018; Szabó, 2010; Yıldırım et al., 2018). Each item utilises a 4-item Likert scale. Higher scores indicate more frequency and severity in the experience of negative emotions.
D. Data Analysis
First, the response rate (n/N) was calculated as a percentage measure, and the details of the participants were described. Second, descriptive statistics (means and standard deviations (SDs)) were computed for the two self-reported questionnaires measures (NZ WHOQOL-BREF and DASS-21). These measures were computed for each of the questionnaire domains with respect to course preference (medicine; other) and gender (male; female). A multivariate analysis of variance (ANOVA) approach was used to assess levels of significance for the independent variables, course preference and gender, with respect to the aforementioned dependent variables.
Lastly, one structural equation model (SEM) was developed to consider the interrelationships among course preference, gender, and QoL and DASS-21 domain measures. This SEM was developed using the software AMOS v25 (Arbuckle, 2017). The primary goodness-of-fit indices used to assess the model fit were inspection of the model chi-square value, root mean square error of approximation (RMSEA), comparative fit index (CFI), and standardised root mean square residual (SRMR). Model fits were considered acceptable if they met the following recommendations: (1) RMSEA < 0.06; (2) SRMR < 0.08; and (3) CFI close to 0.95 or higher (Hu & Bentler, 1998). Additionally, using maximum likelihood bootstrapping with 1,000 samples, regression weights were computed, and bias-corrected 95% confidence intervals were determined (Byrne, 2010).
III. RESULTS
A. Response Rate and Participant Data
Three hundred and sixty-five students (n = 365) fully completed the online survey resulting in a response rate of 29%. The average age of participants was 19 years (SD = 1.84) with 75% of respondents being female. Table 1 provides the demographic profile for the sample, and upon examination, the distributions of the sample data appeared representative of the population profile. In this study, more than 75% of participants stated a preference to study medicine as opposed to other non-medicine health options, which is a rate higher than that found elsewhere (Henning et al., 2017b). The data that support the findings of this study are openly available in Figshare at https://figshare.com/articles/dataset/_/1405 0463 (Henning et al., 2021).
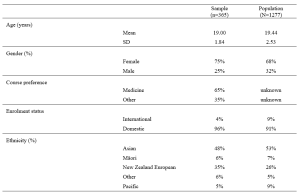
Table 1. Demographic and academic achievement details of the sample versus the population.
The means and standard deviations for the variables of interest are shown in Table 2. The NZ WHOQOL-BREF questionnaire means for these participants are marginally lower than those found elsewhere (Henning et al., 2017b). No comparable New Zealand medical student reference values for the DASS-21 are available for this population. In reference to internal consistency coefficients computed for each of the measures (Table 2), all Cronbach’s alpha values were equal to or greater than 0.70 thus meeting ‘acceptable’ requirements (Field, 2005).
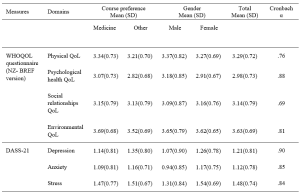
Table 2. Means, standard deviations (SD) and internal consistency scores (Cronbach alpha) of the measures used in the study.
Note: Using a multivariate ANOVA approach, significant differences (p<.05) for course preference (medicine vs. other) were noted for psychological health QoL, environmental QoL, and depression. In addition, significant differences (p<.05) for gender (male vs. female) were noted for psychological health QoL, depression, anxiety and stress.
B. Structured Equation Modelling
Based on previous literature (Dyrbye et al., 2006) and self-determination theory (Katz & Assor, 2007; Ryan & Deci, 2000), an a priori conceptual model was developed and tested using a SEM framework. The primary criterion variable was the students’ course preference (medicine, scored as 1 vs. other, scored as 0). The values obtained for RMSEA, SRMR, and CFI indicated that the model fit was excellent, that is, RMSEA = 0.027, CFI = 0.999, and SRMR = 0.016. As a secondary check, the overall model fit determined by the chi-square (χ2 = 7.626, df=6. p= .267) also indicated the model fitted very well. We noted that some of the error variances within measures of the NZ WHOQOL-BREF and DASS-21 were required to be correlated.
Figure 1 shows the path diagram for all the data collected (n = 365). The path coefficients are shown for significant relationships only (p < .05). The bias-corrected 95% confidence intervals for the regression weights (path coefficients) obtained using the maximum likelihood bootstrapping method were generated (Table 3) to ensure the accuracy and stability of the parameter estimates (Byrne, 2010).
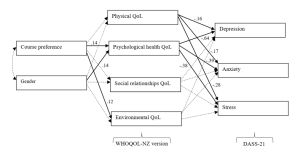
Figure 1. Path diagram of the tested structural equation model for all study participants.
Note. The path standardised regression weight estimates were shown only when statistically significant (p<.05). For non-significant relationships, directive arrows are shown with dashed lines (see Table 3 for details). Errors for all pertinent measures were removed to improve clarity of the figure. Error variances among the WHOQOL- NZ version and DASS-21 domian measures were were allowed to be correlated. No other error variances were correlated. Key fit indices and chi-square calculations were standardised RMR = .016, CFI = .999, RMSEA = .027, χ2 = 7.626, df=6. p= .267
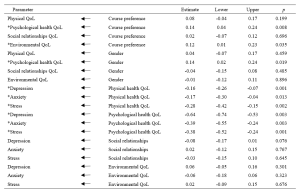
Table 3. Standardised regression weights: Lower and upper ends of bias-corrected 95% confidence intervals of the regression weights of the directional paths of the SEM.
Note. * p<.05
Table 3 and Figure 1 indicated the following relationships. The standardised regression weights determined that course preference significantly predicted psychological health QoL and environmental QoL. More specifically, those students preferring a medical course will likely have higher psychological health QoL and environmental QoL. Gender did not influence course preference but had a significant association with psychological health QoL. In turn, physical QoL and psychological health QoL scores significantly predicted depression, anxiety and stress (DASS-21 measures). The two remaining QoL measures (social relationships QoL and environmental QoL) did not significantly predict the DASS-21 measures.
When inspecting Table 2 and Figure 1, we can make certain assertions related to the differences between the two groups (medical and other students) with respect to QoL and psychological distress. Figure 1 indicates two significant associations between course preference and psychological health QoL and environmental QoL. Therefore, students indicating a preference for enrolling in a medical course were likely to experience greater psychological health QoL and environmental QoL. The findings in Table 2, clarify that students aiming to study medicine have higher levels of QoL in these two domains, compared to students aiming to study in non-medicine courses. In addition, the multivariate analyse indicate that depression is more of a concern for non-medical students than intending medicine students.
IV. DISCUSSION
The known health concerns associated with first year students (Naylor et al., 2018; Tinto, 2009) appear consistent with the current findings. The actual values (Table 2) for three of the four QoL domains from the NZ WHOQOL-BREF -psychological health QoL, social relationships QoL, and environmental QoL – are lower than previously published values for year 4 and 5 students at the same university (Henning et al., 2012), although the physical QoL score was higher. This indicates that year 1 students at this university appear to have relatively lower QoL than their year 4 and 5 peers and are consequently lower than the general population norms, particularly in the areas of psychological health QoL, social relationships QoL, and environmental QoL (Henning et al., 2012). In addition, the values for all domains are lower than those acquired from a 2015 first-year cohort (overall) studying in the same programme (Henning et al., 2017b).
Similarly, the DASS-21 findings (Table 2) show that this group scored higher on the domains of depression and anxiety compared to early career doctors also graduating from the same university (Henning et al., 2014). In comparison to a Malaysian student group, the mean values for the present study show distinct similarity in terms of stress and anxiety scores, but a marked lower score for depression (Yusoff et al., 2013). Therefore, we have provided good evidence to suggest that this group of students, irrespective of choosing either medicine or other as their preferred course option, studying in the BCY programme are experiencing relatively lower levels of QoL and higher levels of psychological distress compared to previous cohorts studying at the same university. However, their experiences may not differ greatly when compared to those students’ psychological distress perceptions in other universities.
In reference to the conceptual model, the findings also confirm that preference for course of study is linked with aspects of QoL. This in turn influences psychological distress, suggesting a feedback loop. Both of these associations were confirmed by the path analysis resulting in an excellent model fit for the SEM (Figure 1). The first part of the model considered how the preferred course option (medicine versus other) could directly impact QoL measures and the second part of the model considered the flow-on (indirect) effects to psychological distress (depression, anxiety and stress).
A. Choosing to Study medicine and Its Impact on Quality of Life
Figure 1 clearly shows that choosing to study medicine has an influence on aspects of QoL, although gender was not found to be significantly correlated with course preference. The decision to choose to study medicine was directly and significantly associated with psychological health QoL and environmental QoL (with higher scores noted for intending medicine students), but did not influence either physical QoL or social relationships QoL. In Table 2, we noted that psychological health QoL and environmental QoL for those vying for a place in the medical programme was higher than students’ scores for other health options (e.g., nursing, pharmacy, or optometry). The direction of the arrows in the model implies that the act of deciding to study medicine is likely influencing QoL on these two domains. These findings can be interpreted in several ways.
First, it is likely that students who aim for admission to medicine may be more psychologically robust to begin with. The psychological health QoL domain of the New Zealand version of the WHOQOL encompasses 10 facets (Krägeloh et al., 2016; WHOQoL Group, 1998). The facets that likely emphasise the difference between those applying for medicine and those applying for another degree are self-esteem, perception of negative or positive feelings, concentration, ability to meet expectation, and management of personal circumstances. In a previous study (Henning et al., 2017b), perceived stress was found to be highly correlated with psychological QoL and also noted to be a strong predictor of course preference (medicine versus other), with potential medical students scoring higher than their other heath professional peers.
Second, the aspects of cognitive capacity, personal management, and mental wellbeing need to be weighed in comparison to environmental QoL (measured in perceived access to resources, i.e., finance, health care, transport, security, technology, and housing) (WHOQoL Group, 1998). The current findings confirm previous research linking course preference to environmental QoL, suggesting that those students who come from affluent and supportive backgrounds will likely have more interest in pursuing a medical degree (Henning et al., 2017b).
B. Impact of Quality of Life on Psychological Distress
The SEM also revealed an interesting flow-on effect suggesting that those students not choosing medicine will have more issues with psychological wellbeing than those choosing to pursue medicine, which translates to greater risk of psychological distress in the form of depression, anxiety and stress for non-medical students. Furthermore, intending medicine students generated significantly lower depression scores than their non-medicine peers. Even though physical QoL is also directly connected with psychological distress factors, this association was not influenced by course preference. Hence, the key issues linked to course preference are related to psychological health QoL, which is incidentally linked to gender. Environmental QoL appears to have no flow-on psychological distress effects.
These findings indicate that some perceptions of QoL are likely linked to choice and ultimately psychological distress factors. The flow-on effect suggests that those students who struggle with psychological health QoL tend to further struggle with psychological distress. The point of difference between the two groups (medical and other) is that the intending medical students appear less affected by depression than their non-medical peers. The concept of choice has been established as a key component in motivation and wellbeing, for example, the perceived expectancies and values regarding a task are influenced by weighing up the benefits and costs associated with the forthcoming task (Katz & Assor, 2007). Hence, in the medical context the preferred choice of medicine likely has a powerful impact on motivation, learning and wellbeing (Katz & Assor, 2007). The current findings indicate that students focussing on medicine have higher psychological health QoL and lower psychological distress (particularly in the area of depression) than non-medicine students in the same year. This may imply that the current programme is more suited to those aiming for a medical career than those heading for a non-medicine health-related vocation, although this proposition requires further investigation.
C. Implications for Learning and Wellbeing
There are two clear implications associated with these results.
First, the findings indicate that intending medical students are more likely to have good access to environmental resources. The elevation of environmental QoL scores for students intending to study medicine as compared to students in other disciplines is consistent with findings reported elsewhere (Collins et al., 1993; Henning et al., 2012; Ng et al., 2009), suggesting that these students likely have better access to the needed resources. Equity arguments regarding selection of medical students is a global concern and impacts areas related to communication, empathetic listening, and shared understandings between clinician and patient (Rao & Flores, 2007). The resources differential suggests a clear argument that students who prefer to study medicine may not equitably mirror the less-resourced population at large and thus may have difficulty relating to large proportions of society. It is important to also emphasise that equity initiatives at the university in which this study was conducted are in place, although the complexity of the issues are multifaceted and may require further development (Curtis et al., 2015; Poole et al., 2009).
Second, the findings in this study clearly indicate that intending medical students are more likely to experience higher levels of psychological health QoL. Therefore, they are more likely to have a different wellbeing outcome than those students who aim for an alternative health sciences career, which may warrant investigating the rationale for placing students aiming for different health professions in one course of study. An argument for placing all health-career students together is likely based on the idea of interprofessional learning (Salamonson et al., 2009). Some of the benefits include improved knowledge gains especially for those students preparing for non-medical courses and positive attitudinal shifts regarding each profession (Carpenter, 1995). The findings in this study revealed that one lecturer was able lecture to 1277 students at one time (using asynchronous technology), suggesting this is a cost effective teaching option. Nonetheless, the findings in this study do indicate that the implication of large classes (or ‘massification’) in reference to wellbeing gains requires further investigation (Hornsby & Osman, 2014).
It has been established that students preferring medicine to other health science options will lead to greater academic attainment. For example, Henning et al. (2017b) reported that those students preferring to pursue medicine attained a bioscience grade average of 6.77 which was significantly higher than the non-medical comparison cohort which attained a grade average of 4.42. Therefore, creating smaller, discipline-specific groups could create more equitable learning, as well as engendering more opportunities for staff-student engagement, more engagement with relevant content, and greater likelihood of motivation for learning (Hornsby & Osman, 2014). However, in the context of pre-medical courses, such as the BCY programme, even though there are clear differences in resulting grade achievement, more research is required to tease out the subtle learning and wellbeing interconnections and to further investigate whether one group is more disadvantaged in their learning than the other (in this case the non-medicine group).
A limitation of this study is the relatively low response rate, although this is comparable with other studies using online questionnaires (Nulty, 2008) and the participants engaged in this study had similar characteristics to the total population (Table 1). Moreover, the response rate is within the range considered acceptable for surveys of representatives of organisations (36%±13%) – a category arguably appropriate for students entering their respective professions (Baruch, 1999). A further limitation of the study is that the research design is cross-sectional suggesting that the links between variables cannot infer temporal causality. Lastly, we acknowledge that it was outside the scope of the study to fully explore some of the speculations raised in this paper, such as whether choice of course of study was influenced by either intrinsic or extrinsic factors (i.e., degree of autonomy).
V. CONCLUSION
The main implication of this study is the direct relationships between course preference (medicine versus other) and psychological health QoL and environmental QoL, as well as the further indirect or flow-on effects to psychological distress via the psychological QoL pathway. Thus, indicating that medical students are not as adversely impacted upon in terms of QoL and psychological distress compared with their non-medicine peers. Lastly, the study findings provide useful debate and scope for further research in the areas of pedagogy, educational equity, career aspiration, and financial cost related to interprofessional education and teaching in large student groups.
Notes on Contributors
Marcus A. Henning is an associate professor in the Centre for Medical and Health Sciences Education at the University of Auckland, New Zealand. MAH was involved in the conceptualisation of the idea, data curation, formal analysis, developing the design of the study, writing the original draft and ongoing editing.
Vanamali Joseph was, at the time of this study, a third year medical student studying in the Faculty of Medical and Health Sciences at the University of Auckland, New Zealand. VJ was involved in the conceptualisation of the idea, data curation, developing the design of the study and ongoing editing.
Roger J. Booth is an associate professor in molecular medicine and pathology, in the Faculty of Medical and Health Sciences at the University of Auckland, New Zealand. RB was involved in the conceptualisation of the idea, data curation, developing the design of the study and ongoing editing.
Christian U. Krägeloh is an associate professor in the Department of Psychology at AUT University, New Zealand. CUK was involved in the conceptualisation of the idea, formal analysis and ongoing editing.
Craig S. Webster is an associate professor in the Centre for Medical and Health Sciences Education at the University of Auckland, New Zealand. CSW was involved in the conceptualisation of the idea, data curation, formal analysis, developing the design of the study, writing the original draft and ongoing editing.
Ethical Approval
Ethics approval for the collection and use of data was obtained from the University of Auckland Human Participants Ethics Committee (Ref. 021985).
Data Availability
The anonymised data that supports the findings of this study are openly available in the Figshare repository, https://figshare.com/articles/dataset/_/14050463
Funding
No funding source required for this study.
Declaration of Interest
The authors declare no conflicts of interest.
References
Al Alwan, I., Al Kushi, M., Tamim, H., Magzoub, M., & Elzubeir, M. (2013). Health sciences and medical college preadmission criteria and prediction of in-course academic performance: A longitudinal cohort study. Advances in Health Sciences Education, 18(3), 427-438. https://doi.org/10.1007/s10459-012-9380-1
Arbuckle, J. L. (2017). IBM® SPSS® Amos™ 25 User’s Guide. https://usermanual.wiki/Document/IBMSPSSAmosUserGuide.2983928102/view
Baruch, Y. (1999). Response rate in academic studies- A comparative analysis. Human Relations, 52(4), 421-438. https://doi.org/10.1177/001872679905200401
Burris, J. L., Brechting, E. H., Salsman, J., & Carlson, C. R. (2009). Factors associated with the psychological well-being and distress of university students. Journal of American College Health, 57(5), 536-544. https://doi.org/10.3200/JACH.57.5.536-544
Byrne, B. M. (2010). Structural Equation Modeling with AMOS: Basic concepts, applications and programming (2nd ed.). Routledge.
Carpenter, J. (1995). Interprofessional education for medical and nursing students: Evaluation of a programme. Medical Education, 29(4), 265-272. https://doi.org/10.1111/j.1365-2923.1995.tb02847.x
Collins, J., Jones, J., & White, G. (1993). Demographic variables in Auckland medical students. New Zealand Medical Journal, 106(960), 306-308.
Curtis, E., Wikaire, E., Jiang, Y., McMillan, L., Loto, R., Airini., & Reid, P. (2015). A tertiary approach to improving equity in health: Quantitative analysis of the Māori and Pacific admission scheme (MAPAS) process, 2008–2012. International Journal for Equity in Health, 14(1), 1-15. https://doi.org/10.1186/s12939-015-0133-7
Dyrbye, L. N., Thomas, M. R., & Shanafelt, T. D. (2006). Systematic review of depression, anxiety, and other indicators of psychological distress among US and Canadian medical students. Academic Medicine, 81(4), 354-373. https://doi.org/10.1097/00001888-200604000-00009
Field, A. P. (2005). Discovering statistics using SPSS : And sex, drugs and rock’n’roll (2nd ed.). SAGE.
Google.com. (2015). Homepage. https://www.google.co.nz/forms/about/
Haist, S. A., Wilson, J. F., Elam, C. L., Blue, A. V., & Fosson, S. E. (2000). The effect of gender and age on medical school performance: An important interaction. Advances in Health Sciences Education: Theory and Practice, 5(3), 197-205. https://doi.org/10.1023/A:1009829611335
Henning, M. A., Joseph, V., Booth, R. J., Krageloh, C. U., & Webster, C. S. (2021). Biomedical students’ course preference and links with quality of life and psychological distress [Data set]. Figshare. https://figshare.com/articles/dataset/_/14050463
Henning, M. A., Krägeloh, C. U., Hawken, S. J., Zhao, Y., & Doherty, I. (2012). The quality of life of medical students studying in New Zealand: A comparison with non-medical students and a general population reference group. Teaching and Learning in Medicine, 24(4), 334-340.https://doi.org/10.1080/10401334.2012.715261
Henning, M. A., Krägeloh, C. U., Booth, R., Hill, E. M., Chen, J., & Webster, C. S. (2017a). Biomedical students in their first year of study: Factors explaining performance in a high stakes examination. Medical Science Educator, 27(4), 633–643. https://doi.org/10.1007/s40670-017-0444-y
Henning, M. A., Krägeloh, C. U., Booth, R., Hill, E. M., Chen, J., & Webster, C. S. (2017b). Profiling potential medical students and exploring determinants of career choice. The Asia Pacific Scholar, 2(1), 7-15. https://doi.org/10.29060/TAPS.2017-2-1/OA1019
Henning, M. A., Krägeloh, C. U., Manalo, E., Doherty, I., Lamdin, R., & Hawken, S. J. (2013). Medical students in early clinical training and achievement motivation: Variations according to gender, enrolment status, and age. Medical Science Educator, 23(1), 6-15. https://doi.org/10.1007/BF03341798
Henning, M. A., Sollers, J., Strom, J. M., Hill, A. G., Lyndon, M. P., Cumin, D., & Hawken, S. J. (2014). Junior doctors in their first year: Mental health, quality of life, burnout and heart rate variability. Perspectives in Medical Education, 3, 136-143. https://doi.org/10.1007/s40037-013-0075-y
Hornsby, D. J., & Osman, R. (2014). Massification in higher education: Large classes and student learning. Higher Education Research & Development, 67(6), 711-719. https://doi.org/10.1007/s10734-014-9733-1
Hu, L.-t., & Bentler, P. M. (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods, 3(4), 424-453. https://doi.org/10.1037/1082-989X.3.4.424
Katz, I., & Assor, A. (2007). When choice motivates and when it does not. Educational Psychology Review, 19(4), 429. https://doi.org/10.1007/s10648-006-9027-y
Krägeloh, C., Henning, M., Hawken, S., Zhao, Y., Shepherd, D., & Billington, R. (2011). Validation of the WHOQOL-BREF quality of life questionnaire for use with medical students. Eductaion for Health, 24(2), 545.
Krägeloh, C. U., Billington, D. R., Hsu, P. H.-C., Feng, X. J., Medvedev, O. N., Kersten, P., Landon, J., & Siegert, R. J. (2016). Ordinal-to-interval scale conversion tables and national items for the New Zealand version of the WHOQOL-BREF. PLOS ONE, 11(11), e0166065. https://doi.org/10.1371/journal.pone.0166065
Le, M. T. H., Tran, T. D., Holton, S., Nguyen, H. T., Wolfe, R., & Fisher, J. (2017). Reliability, convergent validity and factor structure of the DASS-21 in a sample of Vietnamese adolescents. PLOS ONE, 12(7), e0180557. https://doi.org/10.1371/journal.pone.0180557
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335-343.
Medvedev, O. N., Krägeloh, C. U., Titkova, E. A., & Siegert, R. J. (2018). Rasch analysis and ordinal-to-interval conversion tables for the Depression, Anxiety and Stress Scale. Journal of Health 25(10–11), 1374–1383. https://doi.org/10.1177/1359105318755261
Naylor, R., Baik, C., & Arkoudis, S. (2018). Identifying attrition risk based on the first year experience. Higher Education Research & Development, 37(2), 328-342. https://doi.org/10.1080/07294360.2017.1370438
Ng, C. L., Tambyah, P. A., & Wong, C. Y. (2009). Cost of medical education, financial assistance and medical school demographics in Singapore. Singapore Medical Journal, 50(5), 462-467.
Nulty, D. D. (2008). The adequacy of response rates to online and paper surveys: What can be done? Assessment and Evaluation in Higher Education, 33(3), 301-314. https://doi.org/10.1080/02602930701293231
Poole, P. J., Moriarty, H. J., Wearn, A. M., Wilkinson, T. J., & Weller, J. M. (2009). Medical student selection in New Zealand: looking to the future. New Zealand Medical Journal, 122(1306), 88-100.
Ramsbottom-Lucier, M., Johnson, M. M., & Elam, C. L. (1995). Age and gender differences in students’ preadmission qualifications and medical school performances. Academic Medicine, 70(3), 236-239. https://doi.org/10.1097/00001888-199503000-00016
Rao, V., & Flores, G. (2007). Why aren’t there more African-American physicians? A qualitative study and exploratory inquiry of African-American students’ perspectives on careers in medicine. Journal of the National Medical Association, 99(9), 986-993.
Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55(1), 68-78. https://doi.org/10.1037/0003-066X.55.1.68
Salamonson, Y., Everett, B., Koch, J., Wilson, I., & Davidson, P. M. (2009). Learning strategies of first year nursing and medical students: A comparative study. International Journal of Nursing Studies, 46(12), 1541-1547. https://doi.org/10.1016/j.ijnurstu.2009.05.010
Szabó, M. (2010). The short version of the Depression Anxiety Stress Scales (DASS-21): Factor structure in a young adolescent sample. Journal of Adolescence, 33(1), 1-8. https://doi.org/10.1016/j.adolescence.2009.05.014
The NZ WHOQOL Group. (2017). WHOQOL tools. Auckland University of Technology. https://cpcr.aut.ac.nz/new-zealand-whoqol
The University of Auckland. (2019). Biomedical Science. https://www.auckland.ac.nz/en/study/study-options/find-a-study-option/biomedical-science.html
Tinto, V. (2009). Taking student retention seriously: Rethinking the first year of university. FYE curriculum design symposium. Queensland University of Technology, Australia.
Vansteenkiste, M., Lens, W., & Deci, E. L. (2006). Intrinsic versus extrinsic goal contents in self-determination theory: Another look at the quality of academic motivation. Educational Psychologist, 41(1), 19-31. https://doi.org/10.1207/s15326985ep4101_4
Verger, P., Combes, J.-B., Kovess-Masfety, V., Choquet, M., Guagliardo, V., Rouillon, F., & Peretti-Wattel, P. (2009). Psychological distress in first year university students: Socioeconomic and academic stressors, mastery and social support in young men and women. Social Psychiatry and Psychiatric Epidemiology, 44(8), 643-650. https://doi.org/10.1007/s00127-008-0486-y
WHOQoL Group. (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine, 28(3), 551-558. https://doi.org/10.1017/S0033291798006667
Wickramasinghe, D. P., Almeida, I. S., & Samarasekera, D. N. (2019). Depression and stressful life events among medical students during undergraduate career: Findings from a medical school in South Asia. The Asia Pacific Scholar, 4(1), 42-47. https://doi.org/10.29060/TAPS.2019-4-1/OA2025
Yıldırım, A., Boysan, M., & Kefeli, M. C. (2018). Psychometric properties of the Turkish version of the Depression Anxiety Stress Scale-21 (DASS-21). British Journal of Guidance & Counselling, 46(5), 582-595. https://doi.org/10.1080/03069885.2018.1442558
Yusoff, M. S. B., Rahim, A. F. A., Baba, A. A., Ismail, S. B., Pa, M. N. M., & Esa, A. R. (2013). Prevalence and associated factors of stress, anxiety and depression among prospective medical students. Asian Journal of Psychiatry, 6(2), 128-133. https://doi.org/10.1016/j.ajp.2012.09.012
*Marcus A. Henning
The University of Auckland,
Private Bag 92019,
Auckland 1142, New Zealand
Tel: 0064 923 7392
Email: m.henning@auckland.ac.nz
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









