Medical students use, attitudes towards, and knowledge of complementary and alternative medicine: A scoping review
Submitted: 18 January 2021
Accepted: 19 May 2021
Published online: 5 October, TAPS 2021, 6(4), 107-117
https://doi.org/10.29060/TAPS.2021-6-4/OA2470
Sarah Brown & Justin L C Bilszta
Department of Medical Education, Melbourne Medical School, University of Melbourne, Australia
Abstract
Introduction: Use of complementary and alternative medicine (CAM) is popular in the general population and medical practitioners may not be fully equipped in their knowledge of CAM to advise patients appropriately. The aim of this paper was to perform a scoping review of current literature describing undergraduate medical student use, attitudes, and knowledge of CAM as a means of better understanding the educational needs of these students.
Methods: A systematic search of Medline, PubMed and the Education Resources Information Center (ERIC) databases with keywords related to “complementary and alternative medicine” and “undergraduate medical students” for relevant articles published until August 2020.
Results: Of 131 papers identified, 38 underwent full review. It was found 13-80% of medical students use CAM, and overall have a positive attitude towards CAM therapies. Female medical students and those with religiosity had more positive attitudes towards CAM than their male colleagues and those without a religion. Knowledge of CAM is lacking with approximately only half of students feeling they were knowledgeable about CAM therapies. Popular information resources are the Internet and social media, but students expressed they want more teaching of CAM in the undergraduate medical curriculum.
Conclusion: Evidence suggests high usage of CAM amongst undergraduate medical students, and positive attitudes towards CAM therapies; however, knowledge of CAM is poor, and students want more CAM teaching to upskill them in counselling patients interested in CAM therapies. Further areas for research include a better understanding of resources medical students use for their knowledge and how gender and religiosity influence attitudes towards CAM.
Keywords: Undergraduate Medical Student, Complementary and Alternative Medicine, CAM, Attitude, Knowledge, Use
Practice Highlights
- Medical student’s personal use of CAM is significant, with the most popular therapies being massage, meditation and herbal medicine.
- Medical students have a positive attitude towards CAM but potential differences between attitudes of preclinical and clinical student populations exist.
- Medical student’s knowledge of CAM is lacking, and this impacts their ability to advise patients appropriately.
- Medical students want more CAM teaching integrated into their UGME curriculum, and believe conventional western medicine could benefit from CAM methods and ideas.
- Better integration of the principles of EBM rather than teaching related to specific CAM therapies can provide medical students with the skills to critique claims of CAM efficacy.
I. INTRODUCTION
Complementary and alternative medicine (CAM) encompasses a range of health practices including, but not limited to, acupuncture, naturopathy, chiropractic traditional Chinese medicine (TCM), herbal, vitamin & homeopathic therapies (Zollman & Vickers, 1999). Complementary refers to the practice of something alongside conventional Western medicine, whilst alternative refers to the practice of something instead of conventional Western medicine (Zollman & Vickers, 1999).
In comparison to conventional Western medicine, the eclectic range of CAM is often cited as having a poor-quality evidence-base regarding its efficacy (Australian Medical Association, 2018), yet it remains popular with the general public (Frass et al., 2012). With surveys suggesting 10–76% of the public has used CAM (Ernst, 2000; Harris et al., 2012) the demand for CAM is evident. How knowledgeable medical practitioners are, and their attitudes towards CAM, can influence the advice they might provide to patients who seek information about CAM therapies or want to use CAM in lieu of conventional Western medicine. Janamian et al. (2011) have reported general practitioners feel they do not have the education to appropriately advise patients on CAM (Janamian et al., 2011). This may deter patients from seeking guidance from their healthcare provider and result in a breakdown of communication and lack of congruence over health goals (Xue et al., 2007).
Medical students’ insights into their prevailing attitudes and knowledge of CAM can help determine if CAM teaching within undergraduate medical education (UGME) should be expanded to better meet the needs of growing public demand. The last significant review of medical students’ attitudes and knowledge of CAM was published in 2016 (Joyce et al., 2016), and reported overall medical students believed they lacked knowledge of CAM but were generally positive towards CAM education and thought CAM teaching should be incorporated into UGME. What this review did not explore was the rates of CAM use by medical students, and whether this influenced attitudes towards CAM. Importantly, since the publication of Joyce et al’s review, not only have there been additional studies exploring medical students’ use, attitudes and knowledge of CAM, but the increasing use of the Internet and social media as a source of information means it is timely to re-evaluate the findings of this earlier study and determine whether the results presented remain relevant.
We conducted this scoping review of primary studies to evaluate undergraduate medical student use, attitudes, and knowledge of CAM as a means of better understanding the educational needs of these students. The specific research questions were: 1) what is the usage and knowledge of CAM among medical students?; 2) what are medical students’ attitudes towards CAM?; 3) what factors influence medical students’ attitudes towards CAM, and where do they seek information about CAM? and; 4) what are medical students’ views on the current teaching they receive in UGME about CAM?
II. METHODS
This study adopted the “Preferred Reporting Items for Systematic Reviews and Meta-Analysis Extension for Scoping Reviews” (PRISMA-ScR) protocol (Tricco et al., 2018).
A. Search Strategy
Electronic databases Medline (Ovid), PubMed and ERIC were searched for full text articles describing undergraduate medical students use, attitudes, and knowledge of CAM (see Appendix 1). Additional papers were found through a hand search of reference lists of articles identified through the database search. There was no limit on publication date.
B. Selection of Sources
Papers were included if published in English and reported on undergraduate medical students. Papers were excluded if they were not published in English; opinion pieces or review articles; reported on non-undergraduate medical students or; reported on osteopathic medical students. This group was excluded due to the potential bias these students may have due to their medical training including specific CAM teaching.
C. Key Words and Boolean Operators
The search strategy (see Appendix 1) included Boolean operators (AND, NOT, OR), Medical Subject Headings (MeSH) and specific key words.
D. Data Extraction and Charting
Data extraction was performed using a predetermined checklist, and included
- Article details: first author and publication year
- Research aim: purpose of the study
- Method: methods of data collection
- Sample size: number of students invited to participate and the number who responded
- Student CAM use: number of students using CAM, including use of specific therapies and timeframe of use
- Student attitudes/perceptions to CAM: student attitudes to CAM including desire to undertake further education about CAM, beliefs about CAM efficacy, role of CAM in conventional Western medicine and, sources of CAM information
- Influencing factors: factors reported to influence student’s attitudes/perceptions to CAM
- Limitations: identified study limitations
E. Synthesis of Results
Included studies were described by author, publication year, and characteristics described above. Thematic analysis was conducted to identify commonality between included studies. No inferences were made about students’ use, attitudes, or knowledge of CAM if this was not explicitly stated.
Literature searching, title and abstract screening, full text review & data extraction, and charting were undertaken by the 1st author (SB). Where there was uncertainty regarding the aforementioned, these articles were reviewed independently by the 2nd author (JB) and discussed until consensus was reached. The 2nd author also independently reviewed the data extraction and charting results once this process was completed by the 1st author.
III. RESULTS
From the initial search strategy, 131 articles were obtained for screening based on title and abstract. Following screening, 17 duplicate citations were excluded, leaving 114 papers. Abstract and title screening excluded papers focused on pharmacy or nursing students, and those that did not centre on the research questions. Following this, 58 articles underwent full review. Of these, 21 were excluded as they were not in English, did not provide enough detail regarding medical students specifically or focused heavily on medical curricula. The total number of articles included is 38 (see Figure 1); a full version of the outcome harvesting data can be found at https://doi.org/10.6084/m9.figshare.14471250 (Brown & Bilszta, 2021).
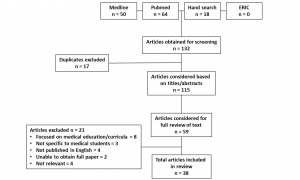
Figure 1: PRISMA Diagram
A. CAM usage
Twenty-two studies assessed CAM usage in medical students (Baugniet et al., 2000; Chaterji et al., 2007; Chez et al., 2001; Ditte et al., 2011; Donald et al., 2010; Flaherty et al., 2015; Frye et al., 2006; Greenfield et al., 2000, 2002; Hegde et al., 2018; Hopper & Cohen, 1998; James et al., 2016; Lie & Boker, 2004, 2006; Nicolao et al., 2010; Oberbaum et al., 2003; Rees et al., 2009; Sadeghi et al., 2016; Samara et al., 2019; Shani-Gershoni et al., 2008; Wong et al., 2006; Yildirim et al., 2010). Rates of usage ranged from 13% to 80% (Chez et al., 2001; Wong et al., 2006). The most common CAM therapy used by medical students was difficult to evaluate due to inconsistent methods of collecting this information with studies either asking students to nominate usage from a predefined list of therapies (Baugniet et al., 2000; Chaterji et al., 2007; Frye et al., 2006; Hegde et al., 2018; James et al., 2016; Lie & Boker, 2004, 2006; Nicolao et al., 2010; Sadeghi et al., 2016; Samara et al., 2019; Shani-Gershoni et al., 2008; Wong et al., 2006; Yildirim et al., 2010); self-report the therapies they had engaged with (Donald et al., 2010; Greenfield et al., 2000, 2002) or; indicating CAM usage without nominating a specific therapy (Chez et al., 2001; Ditte et al., 2011; Flaherty et al., 2015; Hopper & Cohen, 1998; Oberbaum et al., 2003; Rees et al., 2009). The challenge in evaluated CAM usage is highlighted by two separate studies (Lie & Boker, 2004, 2006) which reported a range of practices to be popular including massage, meditation and yoga compared to vitamins, meditation and spirituality, respectively (Lie & Boker, 2004, 2006).
B. CAM perception/attitudes
Overall, the general attitude of medical students towards CAM is positive (Ahmed et al., 2017; Akan et al., 2012; Chaterji et al., 2007; Chez et al., 2001; Ditte et al., 2011; Flaherty et al., 2015; Frye et al., 2006; Furnham & McGill, 2003; Godin et al., 2007; Greenfield et al., 2002, 2006; Hegde et al., 2018; Hopper & Cohen, 1998; James et al., 2016; Lie & Boker, 2004, 2006; Loh et al., 2013; Nicolao et al., 2010; Oberbaum et al., 2003; Perkin et al., 1994; Rees et al., 2009; Sadeghi et al., 2016; Samara et al., 2019; Templeman et al., 2015; Torkelson et al., 2006; Wong et al., 2006; Xie et al., 2020; Yeo et al., 2005) with positive attitudes ranging from 49% to 60% (Ditte et al., 2011; Perkin et al., 1994; Sadeghi et al., 2016). Different methods were used to collect this data including validated measures (for example: (Flaherty et al., 2015; Frye et al., 2006; Rees et al., 2009)), rating scales with various stages of validation (for example: (Ahmed et al., 2017; Oberbaum et al., 2003; Sadeghi et al., 2016; Samara et al., 2019)) or qualitative interviews (for example: (Templeman et al., 2015)).
Differences in the attitude of preclinical and clinical cohorts varied between studies. Akan et al., Furnham & McGill and Syverstad et al. reported preclinical students had a more positive attitude compared to clinical students (Akan et al., 2012; Furnham & McGill, 2003; Syverstad et al., 1999), however others found clinical students were more positive, perhaps due to them receiving more CAM education (Chaterji et al., 2007; Xie et al., 2020). However, multiple studies found no difference between preclinical and clinical cohorts (Ditte et al., 2011; Flaherty et al., 2015; Hopper & Cohen, 1998; Rees et al., 2009). Additionally, all studies bar one (Hübner et al., 2012) asked students to consider attitudes and perceptions in relation to ‘…their clinical practice…’ rather than associated with a specific clinical context or medical condition.
Attitudes towards specific CAM therapies demonstrated acupuncture received consistent positive perceptions ranging from 77% to above 90% (Loh et al., 2013; Torkelson et al., 2006; Yeo et al., 2005). Other therapies with consistent positive perceptions include massage and meditation, with more than 70% of medical students feeling positively towards these practices (Furnham & McGill, 2003; Loh et al., 2013; Torkelson et al., 2006). Conversely, Greenfield et al. and Loh et al. both found homeopathy had the most negative perception from students (Greenfield et al., 2006; Loh et al., 2013). Interestingly, studies indicate ambivalence towards chiropractic practice, with some reporting positive attitudes whilst others reported negative attitudes (Greenfield et al., 2006; Loh et al., 2013). When asked about the integration of CAM with conventional Western medicine, there was overwhelming belief from medical students that benefits may come from applying these practices together. Ahmed et al. and Chez et al. reported a large percentage of their cohorts believed conventional Western medicine could benefit from CAM methods and ideas (67% and 89%, respectively) (Ahmed et al., 2017; Chez et al., 2001). Similar findings have been reported by others, with the percentage of students wanting the integration of CAM and conventional Western medicine ranging from 71% to 92% (Chez et al., 2001; Hopper & Cohen, 1998; Lie & Boker, 2004; Loh et al., 2013; Nicolao et al., 2010; Torkelson et al., 2006; Xie et al., 2020; Yeo et al., 2005).
An important question to consider when evaluating medical student knowledge and attitudes towards CAM is whether they believe CAM works. This question arose frequently in the reviewed literature, with investigators trying to determine if there was congruence between having a positive perception of CAM and belief in its efficacy. When asked if participants found the results of CAM were mainly due to the placebo effect, there were mixed findings with 39-59% of medical students agreeing the CAM efficacy was mainly due to the placebo effect (Baugniet et al., 2000; Nicolao et al., 2010; Yeo et al., 2005; Yildirim et al., 2010). Interestingly, recent studies by Xie et al. and Samara et al. reported only 10% and 35%, respectively, believed CAM efficacy was due to the placebo effect (Samara et al., 2019; Xie et al., 2020). Whether this is simply a cohort effect or a reflection that over time students may be becoming less sceptical of CAM, is unable to be confirmed.
Factors that influence attitudes towards CAM should be considered as they may alter how medical students perceive CAM therapies. The most frequent influence reported was gender, with female medical students overall tending to have a more positive attitude than male colleagues (Akan et al., 2012; Chaterji et al., 2007; Ditte et al., 2011; Donald et al., 2010; Flaherty et al., 2015; Frye et al., 2006; Furnham & McGill, 2003; Godin et al., 2007; Greenfield et al., 2002, 2006; Hübner et al., 2012; Oberbaum et al., 2003; Rees et al., 2009; Schmidt et al., 2005; Xie et al., 2020). Interestingly, Ditte et al. found male medical students feared the social stigma of using CAM more than female students (45% vs 36%) and Donald et al. reported male students were more likely to be more sceptical of CAM than female students (50% vs 44%) (Ditte et al., 2011; Donald et al., 2010).
Religion may also influence attitudes to CAM. Yeo et al. reported nearly two thirds of their cohort believed spiritual/religious beliefs influenced attitudes towards CAM (Yeo et al., 2005). Furnham & McGill reported similar findings as female students and students that rated themselves higher religiously, were more eager for CAM to be on the curriculum compared to males and those who were less religious (Furnham & McGill, 2003). In contrast, Loh et al. reported students with no religion tended to be less interested in CAM (Loh et al., 2013).
C. CAM knowledge
The included studies suggest approximately only half of medical students felt knowledgeable about CAM (Hopper & Cohen, 1998; James et al., 2016; Sadeghi et al., 2016; Shani-Gershoni et al., 2008) and the most common individual therapies students were subjectively knowledgeable in were massage (Baugniet et al., 2000; Chez et al., 2001; Frye et al., 2006; Furnham & McGill, 2003), acupuncture (Akan et al., 2012; Nicolao et al., 2010; Sadeghi et al., 2016; Yeo et al., 2005), chiropractic (Baugniet et al., 2000; Chez et al., 2001; Frye et al., 2006) and herbal medicine (Akan et al., 2012; Baugniet et al., 2000; Chez et al., 2001). It is clear, however, medical students still perceive significant gaps in their knowledge of CAM. Nicolao et al. reported although students indicated acupuncture and homeopathy as their most knowledgeable areas, this was only for a minority of the cohort (34% and 43%, respectively) and the majority of students felt their level of knowledge, and therefore ability to appropriately advise patients, was poor (Nicolao et al., 2010). In one Australian study, investigators found out of ten common CAM therapies (acupuncture, chiropractic, herbal medicine, homeopathy, hypnosis, massage, meditation, naturopathy, reflexology and spiritual healing) 56% of their cohort had no knowledge of any of these therapies (Hopper & Cohen, 1998).
The Internet appears to be a popular avenue for finding CAM information with Lie and Boker reporting 81% of their cohort used online resources as their main information source (Lie & Boker, 2004). Although the specific online resources used were not described, journals, books and health databases were used less frequently in comparison (41%, 38% and 28%, respectively) (Lie & Boker, 2004). A study of Chinese medical students with CAM teaching integrated into their UGME, found their cohort’s main source of information was from teachers, making up 91% with only 2% using the Internet (Xie et al., 2020). Samara et al. reported 73% of their cohort used social media as their main source of information (Samara et al., 2019).
It is clear medical students want more teaching about CAM in their UGME. Flaherty et al. reported just over two thirds of students across all year levels had a desire to study CAM, however, there was a positive correlation between those students who wanted more teaching and a positive attitude towards CAM (Flaherty et al., 2015). Similar findings were reported by Perkins et al. and Frye et al. with approximately 85% of clinical and preclinical students believing they should learn about CAM in UGME (Frye et al., 2006; Perkin et al., 1994). In terms of this would look like in the curriculum, Greenfield et al. reported 67% wanted to study the theory, with Greiner et al. and Yeo et al. finding 72% and 86%, respectively, wanted clinical exposure (Greenfield et al., 2006; Greiner et al., 2000; Yeo et al., 2005). In semi-structured qualitative interviews of Australian medical students, CAM education was considered important regardless of specialisation and CAM literacy was an ethical responsibility (Templeman et al., 2015).
IV. DISCUSSION
In this Discussion, we provide commentary on our findings, consider how these might be applied to the design of UGME curriculum, and suggest areas of further research.
In the current study, we found a significant number of medical students use CAM, however reported rates varied considerably, and our analysis suggests inconsistency in approaches used to assess CAM use may explain the observed differences. As highlighted, data collection was split between those studies that provided a predefined list of specific CAM therapies, with a limited number of response options, and the exact therapies between papers incongruent; those that allowed students to self-report usage and; those indicating CAM usage without nominating a specific therapy (see Table 1). Cultural differences may also explain usage variation; for example, the high use of yoga in Indian medical students (Hegde et al., 2018), TCM in Chinese medical students (Wong et al., 2006) and, traditional Iranian medicine in Iranian medical students (Sadeghi et al., 2016).
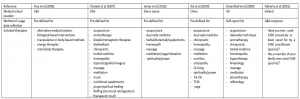
Table 1. Example of the differing methods used to collect student CAM usage data. Data collection of medical student CAM usage was split between those studies that provided a predefined list of specific CAM therapies; those that allowed students to self-report usage and; those indicating CAM usage without nominating a specific therapy. The above examples highlight the inconsistent approaches to collecting this information.
Overall, the general attitude of medical students towards CAM was positive, but differences were noted between preclinical and clinical students, and what exposure students had had to CAM teaching. There is evidence positive attitudes to CAM decline after the preclinical period (Akan et al., 2012; Furnham & McGill, 2003; Syverstad et al., 1999) and this might be due, in part, to the influence of clinical peers, medical school role models or a preference for students new to clinical learning utilizing recently acquired conventional clinical skills. Further work is required to fully elucidate how attitudes to CAM mature as students move from preclinical to clinical learning, are exposed to the application of conventional and CAM practices in different patient encounters and develop skills in the application of evidence-based medicine (EBM).
Two significant factors influencing attitudes to CAM were gender and religion, and these were also identified previously (Joyce et al., 2016).
Whilst medical students as a whole seem to have a positive attitude towards CAM, female students hold more positive attitudes than their male colleagues. There is evidence to suggest this difference is due to higher rates of scepticism around the CAM efficacy in male students (Donald et al., 2010) and fear of social stigma from using CAM (Ditte et al., 2011). There is a noted body of evidence demonstrating similar gender differences in general (Bishop & Lewith, 2010; Kristoffersen et al., 2014) and specific patient populations (Alwhaibi et al., 2019; Alwhaibi & Sambamoorthi, 2016; Barraco et al., 2005; Bell et al., 2006; Jawahar et al., 2012), so it is not surprising this is reflected in medical student cohorts; this is an area for further exploration.
Research within general and specific patient populations into the association between religiosity (the practices of organised religion and the outward expression of belief in a divine being) and spirituality (the personal and emotional expression that arises from searching for a divine being) and CAM utilisation has examined these as a single construct (Heller et al., 2020; McCurdy et al., 2003; Pedersen et al., 2013), or as separate entities (Ben-Arye et al., 2012; Ellison et al., 2012; Hsiao et al., 2008). An added challenge (Ellison et al., 2012; Hsiao et al., 2008) has been attempts to tease out use of religious/spiritual forms of CAM (eg self-prayer, group prayer, or healing rituals) from use of non-religious/nonspiritual forms (eg herbs, supplements, and mind–body techniques). As a result, it remains ambiguous whether religiosity and spiritually are associated with increased CAM utilisation. The results presented here and by others (Joyce et al., 2016) suggests within medical student cohorts an association might be present however the nature remains unclear. What needs to be explored is the intersection between conventional UGME, attitudes to CAM and student’s religious and spiritual beliefs.
Several studies reported most students did not feel knowledgeable about CAM and this impacted their ability to advise patients appropriately (Chaterji et al., 2007; Loh et al., 2013; Torkelson et al., 2006). When evaluating student’s knowledge of CAM, an important limitation is the ways in which knowledge was evaluated. Most studies used self-report, rather than objective, knowledge measures. The only study which attempted to use an objective measure reported the average knowledge of CAM was ‘poor’ (Samara et al., 2019). There is, however, a clear indication medical students want more CAM teaching integrated into UGME. This is relevant as there is evidence CAM users frequently neglect to disclose their usage to their treating health professional (Chao et al., 2008; Davis et al., 2012; Thomson et al., 2012). Foley et al. (2019) identified several factors influencing this including, importantly in this context, perceptions of health professional’s knowledge of CAM and lack of knowledge is considered a barrier to discussions of CAM use during clinical consultations (Foley et al., 2019).
Although medical students believe conventional Western medicine could benefit from CAM methods and ideas, an important caveat to this finding is it does not consider how they feel about specific CAM therapies. For example, would medical students think conventional Western medicine could benefit from integrating herbal medicine or homeopathy approaches, compared to osteopathy or acupuncture? Given the diversity of CAM, it is arguably unfeasible (Wetzel et al., 1998) to teach students about each individual therapy, so an EBM teaching model equipping students with skills needed to critically appraise evidence presents a potential solution, and several medical schools have designed curricular in this way (Bailey et al., 2015; Forjuoh et al., 2003; Hassed, 2004; Jeffries, 2001; Mahapatra et al., 2017; Owen & Lewith, 2001; Perlman & Stagnaro-Green, 2010). This addresses a thematically overwhelming and resource intensive area of medical education where learned knowledge and skills can be adapted for differing CAM therapies.
Only three studies (Lie & Boker, 2004; Samara et al., 2019; Xie et al., 2020) specifically explored how medical students use digital resources to supplement formal CAM teaching, so this is a clear direction for further research. It is important medical students have access to high quality evidence-based information and the skills to determine the validity of evidence presented on digital platforms. Whilst there is evidence to demonstrate resources such as blogs, social networking sites and online support groups are useful platforms for health education, social connection and experience sharing, they are at significant risk of misinformation and mischaracterisation of CAM (Delgado-López & Corrales-García, 2018; Molassiotis & Xu, 2004). Sharma et al. (2016) have underscored the challenges in developing approaches for identifying the reliability of CAM-related information on the Internet, which may not be supported by a reliable evidence-base (Sharma et al., 2016). This means medical students require skills to critique claims related to CAM efficacy for their own education needs, but also so they can appropriately counsel patients. As advocated, an EBM teaching model would provide students with the skills to critique claims of CAM efficacy as well as empower patients to make informed decisions relevant to their health needs.
V. LIMITATIONS OF THE STUDY
As we did not conduct a systematic review of the literature, we are unable to draw any conclusions about the quality of the included studies. We excluded non-English studies, and this potentially creates a gap in the literature and may have altered the findings as CAM use, attitudes and knowledge may be different in non-English speaking countries (for example, the high use of acupuncture or Traditional Chinese medicine in Asian countries). The lack of consistency in data related to medical student use, attitudes and knowledge of CAM therapies is reflected in its heterogeneity. This makes generalisations related to ‘medical students’, even within the same medical school or UGME curriculum, difficult. Despite this significant limitation, the diversity of reported outcomes reflects important contextual differences in medical programs, and medical student cohorts, across the globe.
VI. CONCLUSION
Overall, medical students have a positive attitude towards CAM, with significant influencing factors being gender and religion, and potential differences between preclinical and clinical cohorts. The included literature indicates medical students’ personal use of CAM is significant, with therapies such as massage, meditation and herbal medicine being more popular than others. It is clear medical students’ CAM knowledge is lacking and integration of the principles of EBM may be beneficial in addressing this, ultimately leading to better educated doctors who have better relationships with their patients.
Notes on Contributors
JB: conceptualised the review; JB, SB: designed the search strategy; SB: conducted the search and screened the literature; JB, SB: reviewed the included studies; SB: analysed the data; JB: drafted the manuscript; JB, SB: critically revised the manuscript. All authors had full access to all study data, read and approved the final version of the manuscript.
Ethical Approval
As all the data were retrieved from public databases, this study did not require institutional review board approval.
Data Availability
The data that support the findings of this study are openly available in Figshare repository, https://doi.org/10.6084/m9.figshare.14471250. The data extraction sheet used during the current study is available from the corresponding author on request. All data is based on published studies.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Declaration of Interest
None of the listed authors have financial and personal relationships with organisations or people that could inappropriately influence their work.
References
Ahmed, S. M., Al-Mansour, M. A., Mohamed, E. Y., Medani, K. A., Abdalla, S. M., & Mahmoud, W. S. (2017). Medical Students’ Opinion Toward the Application of Complementary and Alternative Medicine in Healthcare. Saudi Journal of Medicine & Medical Sciences, 5(1), 20-25. https://doi.org/10.4103/1658-631X.194255
Akan, H., Izbirak, G., Kaspar, E. C., Kaya, C. A., Aydin, S., Demircan, N., Bucaktepe, P. G., Ozer, C., Sahin, H. A., & Hayran, O. (2012). Knowledge and attitudes towards complementary and alternative medicine among medical students in Turkey. BMC Complementary & Alternative Medicine, 12, 115. https://doi.org/10.1186/1472-6882-12-115
Alwhaibi, M., AlRuthia, Y., & Meraya, A. (2019). Gender differences in the prevalence of complementary and alternative medicine utilization among adults with arthritis in the United States. Evidence-Based Complementary & Alternative Medicine: eCAM. https://doi.org/10.1155/2019/8739170
Alwhaibi, M., & Sambamoorthi, U. (2016). Sex differences in the use of complementary and alternative medicine among adults with multiple chronic conditions. Evidence-Based Complementary & Alternative Medicine: eCAM. https://doi.org/10.1155/2016/2067095
Australian Medical Association. (2018). AMA Position Statement, Complementary Medicine. https://ama.com.au/position-statement/ama-position-statement-complementary-medicine-2018
Bailey, M. L., Chudgar, S. M., Engle, D. L., Moon, S. D., Grochowski, C. O., & Clay, A. S. (2015). The impact of a mandatory immersion curriculum in integrative medicine for graduating medical students. Explore (NY), 11(5), 394-400. https://doi.org/10.1016/j.explore.2015.07.003
Barraco, D., Valencia, G., Riba, A., Nareddy, S., Draus, C., & Schwartz, S. (2005). Complementary and alternative medicine (CAM) use patterns and disclosure to physicians in acute coronary syndromes patients. Complementary Therapies in Medicine, 13(1), 34-40. https://doi.org/ 10.1016/j.ctim.2005.02.003
Baugniet, J., Boon, H., & Ostbye, T. (2000). Complementary/alternative medicine: comparing the view of medical students with students in other health care professions. Family Medicine, 32(3), 178-184.
Bell, R., Suerken, C., Grzywacz, J., Lang, W., Quandt, S., & Arcury, T. (2006). Complementary and alternative medicine use among adults with diabetes in the United States. Alternative Therapies in Health and Medicine, 12, 16-22.
Ben-Arye, E., Schiff, E., Vintal, H., Agour, O., Preis, L., & Steiner, M. (2012). Integrating complementary medicine and supportive care: Patients’ perspectives toward complementary medicine and spirituality. Journal of Alternative and Complementary Medicine, 18(9), 824-831. https://doi.org/10.1089/acm.2011.0327
Bishop, F., & Lewith, G. (2010). Who uses CAM? A narrative review of demographic characteristics and health factors associated with CAM use. Evidence-Based Complementary & Alternative Medicine: eCAM, 7(1), 11-28. https://doi.org/10.1093/ecam/nen023
Brown, S., & Bilszta, J. L. C. (2021). Medical students use, attitudes towards, and knowledge of complementary and alternative medicine: A scoping review [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.14471250
Chao, M., Wade, C., & Kronenberg, F. (2008). Disclosure of complementary and alternative medicine to conventional medical providers: Variation by race/ethnicity and type of CAM. Journal of the National Medical Association, 100(11), 1341-1349. https://doi.org/10.1016/s0027-9684(15)31514-5
Chaterji, R., Tractenberg, R. E., Amri, H., Lumpkin, M., Amorosi, S. B., & Haramati, A. (2007). A large-sample survey of first- and second-year medical student attitudes toward complementary and alternative medicine in the curriculum and in practice. Alternative Therapies in Health & Medicine, 13(1), 30-35.
Chez, R. A., Jonas, W. B., & Crawford, C. (2001). A survey of medical students’ opinions about complementary and alternative medicine. American Journal of Obstetrics and Gynecology, 185(3), 754-757. https://doi.org/10.1067/mob.2001.117484
Davis, E. L., Oh, B., Butow, P. N., Mullan, B. A., & Clarke, S. (2012). Cancer patient disclosure and patient-doctor communication of complementary and alternative medicine use: A systematic review. The Oncologist, 17(11), 1475-1481. https://doi.org/10.1634/theoncologist.2012-0223
Delgado-López, P., & Corrales-García, E. (2018). Influence of Internet and social media in the promotion of alternative oncology, cancer quackery, and the predatory publishing phenomenon. Cureus, 10(5), e2617. https://doi.org/10.7759/cureus.2617
Ditte, D., Schulz, W., Ernst, G., & Schmid-Ott, G. (2011). Attitudes towards complementary and alternative medicine among medical and psychology students. Psychology, Health & Medicine, 16(2), 225-237. https://doi.org/10.1080/13548506.2010.532559
Donald, G. K., Mackereth, P., & Tobin, I. (2010). Medical students and acupuncture: A short sharp placement experience! Acupuncture Medicine, 28(1), 12-15. https://doi.org/10.1136/aim.2009.001602
Ellison, C. G., Bradshaw, M., & Roberts, C. A. (2012). Spiritual and religious identities predict the use of complementary and alternative medicine among US adults. Preventive Medicine, 54(1), 9-12. https://doi.org/10.1016/j.ypmed.2011.08.029
Ernst, E. (2000). Prevalence of use of complementary/alternative medicine: A systematic review. Bulletin of the World Health Organization, 78(2), 252-257.
Flaherty, G., Fitzgibbon, J., & Cantillon, P. (2015). Attitudes of medical students toward the practice and teaching of integrative medicine. Journal of Integrative Medicine, 13(6), 412-415. https://doi.org/10.1016/s2095-4964(15)60206-0
Foley, H., Steel, A., Cramer, H., Wardle, J., & Adams, J. (2019). Disclosure of complementary medicine use to medical providers: A systematic review and meta-analysis. Scientific Reports, 9(1573). https://doi.org/10.1038/s41598-018-38279-8
Forjuoh, S. N., Rascoe, T. G., Symm, B., & Edwards, J. C. (2003). Teaching medical students complementary and alternative medicine using evidence-based principles. The Journal of Alternative & Complementary Medicine, 9(3), 429-439.
Frass, M., Strassl, R. P., Friehs, H., Müllner, M., Kundi, M., & Kaye, A. D. (2012). Use and acceptance of complementary and alternative medicine among the general population and medical personnel: A systematic review. Ochsner Journal, 12(1), 45-56.
Frye, A. W., Sierpina, V. S., Boisaubin, E. V., & Bulik, R. J. (2006). Measuring what medical students think about complementary and alternative medicine (CAM): A pilot study of the complementary and alternative medicine survey. Advances in Health Sciences Education, 11(1), 19-32. https://doi.org/10.1007/s10459-005-1587-y
Furnham, A., & McGill, C. (2003). Medical students’ attitudes about complementary and alternative medicine. The Journal of Alternative & Complementary Medicine, 9(2), 275-284. https://doi.org/10.1089/10755530360623392
Godin, G., Beaulieu, D., Touchette, J. S., Lambert, L. D., & Dodin, S. (2007). Intention to encourage complementary and alternative medicine among general practitioners and medical students. Behavioral Medicine, 33(2), 67-77.
Greenfield, S. M., Brown, R., Dawlatly, S. L., Reynolds, J. A., Roberts, S., & Dawlatly, R. J. (2006). Gender differences among medical students in attitudes to learning about complementary and alternative medicine. Complementary Therapies in Medicine, 14(3), 207-212. https://doi.org/10.1016/j.ctim.2005.12.001
Greenfield, S. M., Innes, M. A., Allan, T. F., & Wearn, A. M. (2002). First year medical students’ perceptions and use of complementary and alternative medicine. Complementary Therapies in Medicine, 10(1), 27-32. https://doi.org/10.1054/ctim.2002.0501
Greenfield, S. M., Wearn, A. M., Hunton, M., & Innes, M. A. (2000). Considering the alternatives: A special study module in complementary therapy. Complementary Therapies in Medicine, 8(1), 15-20.
Greiner, K. A., Murray, J. L., & Kallail, K. J. (2000). Medical student interest in alternative medicine. The Journal of Alternative & Complementary Medicine, 6(3), 231-234. https://doi.org/10.1089/acm.2000.6.231
Harris, P. E., Cooper, K. L., Relton, C., & Thomas, K. J. (2012). Prevalence of complementary and alternative medicine (CAM) use by the general population: A systematic review and update. International Journal of Clinical Practice, 66(10), 924–939. https://doi.org/10.1111/j.1742-1241.2012.02945.x
Hassed, C. S. (2004). Bringing holism into mainstream biomedical education. The Journal of Alternative and Complementary Medicine, 10(2), 405-407. https://doi.org/10.1089/107555304323062428
Hegde, S. V., Rao, S. K., Menezes, R. G., Kotian, S. M., & Shetty, S. (2018). Knowledge, attitude, and practice of yoga in medical students: Assessment of anthropometry and lifestyle factors. International Journal of Yoga Therapy, 28(1), 9-14. https://doi.org/10.17761/2018-00005r1
Heller, T., Kloos, C., Mueller, N., Roemelt, J., Keinki, C., Wolf, G., Mueller, U. A., & Huebner, J. (2020). Complementary and alternative medicine is positively associated with religiousness/ spirituality. Journal of Complementary & Integrative Medicine, Advance online publication. https://doi.org/10.1515/jcim-2018-0023
Hopper, I., & Cohen, M. (1998). Complementary therapies and the medical profession: A study of medical students’ attitudes. Alternative Therapies in Health and Medicine, 4(3), 68-73.
Hsiao, A.-F., Wong, M. D., Miller, M. F., Ambs, A. H., Goldstein, M. S., Smith, A., Ballard-Barbash, R., Becerra, L. S., Cheng, E. M., & Wenger, N. S. (2008). Role of religiosity and spirituality in complementary and alternative medicine use among cancer survivors in California. Integrative Cancer Therapies, 7(3), 139-146. https://doi.org/10.1177/1534735408322847
Hübner, J., Wicker, S., & Münstedt, K. (2012). Survey of students regarding their attitudes toward complementary and alternative medicine in oncology. Forschende Komplementarmedizin, 19(6), 319-321. https://doi.org/10.1159/000345973
James, P. B., Bah, A. J., & Kondorvoh, I. M. (2016). Exploring self-use, attitude and interest to study complementary and alternative medicine (CAM) among final year undergraduate medical, pharmacy and nursing students in Sierra Leone: A comparative study. BMC Complementary & Alternative Medicine, 16, 121. https://doi.org/10.1186/s12906-016-1102-4
Janamian, T., O’Rourke, P., Myers, S. P., & Eastwood, H. (2011). Information resource needs and preference of Queensland general practitioners on complementary medicines: Result of a needs assessment. Evidence-Based Complementary & Alternative Medicine: eCAM, https://doi.org/10.1155/2011/810908
Jawahar, R., Yang, S., Eaton, C. B., McAlindon, T., & Lapane, K. L. (2012). Gender-specific correlates of complementary and alternative medicine use for knee osteoarthritis. Journal of Women’s Health, 21(10), 1091-1099. https://doi.org/10.1089/jwh.2011.3434
Jeffries, W. B. (2001). A fourth-year elective course in alternative medicine. Academic Medicine, 76(5), 525-526. https://doi.org/10.1097/00001888-200105000-00060
Joyce, P., Wardle, J., & Zaslawski, C. (2016). Medical student attitudes towards complementary and alternative medicine (CAM) in medical education: A critical review. Journal of Complementary & Integrative Medicine, 13(4), 333-345. https://doi.org/10.1515/jcim-2014-0053
Kristoffersen, A. E., Stub, T., Salamonsen, A., Musial, F., & Hamberg, K. (2014). Gender differences in prevalence and associations for use of CAM in a large population study. BMC Complementary & Alternative Medicine, 14, 463. https://doi.org/10.1186/1472-6882-14-463
Lie, D., & Boker, J. (2004). Development and validation of the CAM Health Belief Questionnaire (CHBQ) and CAM use and attitudes amongst medical students. BMC Medical Education, 4, 2. https://doi.org/10.1186/1472-6920-4-2
Lie, D. A., & Boker, J. (2006). Comparative survey of Complementary and Alternative Medicine (CAM) attitudes, use, and information-seeking behaviour among medical students, residents & faculty. BMC Medical Education, 6, 58. https://doi.org/10.1186/1472-6920-6-58
Loh, K. P., Ghorab, H., Clarke, E., Conroy, R., & Barlow, J. (2013). Medical students’ knowledge, perceptions, and interest in complementary and alternative medicine. The Journal of Alternative & Complementary Medicine, 19(4), 360-366. https://doi.org/10.1089/acm.2012.0014
Mahapatra, S., Bhagra, A., Fekadu, B., Li, Z., Bauer, B. A., & Wahner-Roedler, D. L. (2017). Incorporation of integrative medicine education into undergraduate medical education: A longitudinal study. Journal of Integrative Medicine, 15(6), 442-449. https://doi.org/10.1016/s2095-4964(17)60367-4
McCurdy, E. A., Spangler, J. G., Wofford, M. M., Chauvenet, A. R., & McLean, T. W. (2003). Religiosity is associated with the use of complementary medical therapies by pediatric oncology patients. Journal of Pediatric Hematology Oncology, 25(2), 125-129.
Molassiotis, A., & Xu, M. (2004). Quality and safety issues of web-based information about herbal medicines in the treatment of cancer. Complementary Therapies in Medicine, 12(4), 217-227. https://doi.org/10.1016/j.ctim.2004.09.005
Nicolao, M., Täuber, M. G., Marian, F., & Heusser, P. (2010). Complementary medicine courses in Swiss medical schools: Actual status and students’ experience. Swiss Medical Weekly, 140(3-4), 44-51.
Oberbaum, M., Notzer, N., Abramowitz, R., & Branski, D. (2003). Attitude of medical students to the introduction of complementary medicine into the medical curriculum in Israel. Israel Medical Association Journal, 5(2), 139-142.
Owen, D., & Lewith, G. T. (2001). Complementary and alternative medicine (CAM) in the undergraduate medical curriculum: the Southampton experience. Medical Education, 35(1), 73-77. https://doi.org/10.1046/j.1365-2923.2001.00762.x
Pedersen, C. G., Christensen, S., Jensen, A. B., & Zachariae, R. (2013). In God and CAM we trust. Religious faith and use of complementary and alternative medicine (CAM) in a nationwide cohort of women treated for early breast cancer. Journal of Religion and Health, 52(3), 991-1013. https://doi.org/10.1007/s10943-012-9569-x
Perkin, M. R., Pearcy, R. M., & Fraser, J. S. (1994). A comparison of the attitudes shown by general practitioners, hospital doctors and medical students towards alternative medicine. Journal of the Royal Society of Medicine, 87(9), 523-525.
Perlman, A., & Stagnaro-Green, A. (2010). Developing a complementary, alternative, and integrative medicine course: One medical school’s experience. Journal of Alternative & Complementary Medicine, 16(5), 601-605. https://doi.org/10.1089/acm.2009.0276
Rees, C. E., Wearn, A. M., Dennis, I., Amri, H., & Greenfield, S. M. (2009). Medical students’ attitudes to complementary and alternative medicine: Further validation of the IMAQ and findings from an international longitudinal study. Medical Teacher, 31(2), 125-132. https://doi.org/10.1080/01421590802139724
Sadeghi, M., Rabiepoor, S., Forough, A. S., Jabbari, S., & Shahabi, S. (2016). A survey of medical students’ knowledge and attitudes toward complementary and alternative medicine in Urmia, Iran. Journal of Evidence-Based Integrative Medicine, 21(4), 306-310. https://doi.org/10.1177/2156587215605751
Samara, A. M., Barabra, E. R., Quzaih, H. N., & Zyoud, S. H. (2019). Use and acceptance of complementary and alternative medicine among medical students: A cross sectional study from Palestine. BMC Complementary & Alternative Medicine, 19(1), 78. https://doi.org/10.1186/s12906-019-2492-x
Schmidt, K., Rees, C., Greenfield, S., Wearn, A. M., Dennis, I., Patil, N. G., Amri, H., & Boon, H. (2005). Multischool, international survey of medical students’ attitudes toward “holism”. Academic Medicine, 80(10), 955-963. https://doi.org/10.1097/00001888-200510000-00017
Shani-Gershoni, Z., Freud, T., Press, Y., & Peleg, R. (2008). Knowledge and attitudes of internists compared to medical students regarding acupuncture. Israel Medical Association Journal, 10(3), 219-223.
Sharma, V., Holmes, J., & Sarkar, I. (2016). Identifying complementary and alternative medicine usage information from internet resources. A systematic review. Methods of Information in Medicine, 55(4), 322-332. https://doi.org/10.3414/ME15-01-0154
Syverstad, D., Norheim, A., & Fonnebo, V. (1999). Changes in medical students’ attitudes toward acupuncture: The possible impact of role models. Education for Health: Change in Learning & Practice, 12(2), 195-210.
Templeman, K., Robinson, A., & McKenna, L. (2015). Student identification of the need for complementary medicine education in Australian medical curricula: A constructivist grounded theory approach. Complementary Therapies in Medicine, 23(2), 257-264. https://doi.org/10.1016/j.ctim.2015.02.002
Thomson, P., Jones, J., Evans, J. M., & Leslie, S. L. (2012). Factors influencing the use of complementary and alternative medicine and whether patients inform their primary care physician. Complementary Therapies in Medicine, 20(1-2), 45-53. https://doi.org/10.1016/j.ctim.2011.10.001
Torkelson, C., Harris, I., & Kreitzer, M. J. (2006). Evaluation of a complementary and alternative medicine rotation in medical school. Alternative Therapies in Health and Medicine, 12(4), 30-34.
Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D. J., Horsley, T., Weeks, L., Hempel, S., Akl, E. A., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M. G., Garritty, C., … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMAScR): Checklist and explanation. Annals of Internal Medicine, 169, 467-473. https://doi.org/10.7326/M18-0850
Wetzel, M. S., Eisenberg, D. M., & Kaptchuk, T. J. (1998). Courses involving complementary and alternative medicine at US medical schools. Journal of the American Medical Association, 280(9). https://doi.org/10.1001/jama.280.9.784
Wong, W. C., Lee, A., Wong, S. Y., Wu, S. C., & Robinson, N. (2006). Strengths, weaknesses, and development of Traditional Chinese Medicine in the health system of Hong Kong: Through the eyes of future Western doctors. Journal of Alternative & Complementary Medicine, 12(2), 185-189; 191-182. https://doi.org/10.1089/acm.2006.12.185
Xie, H., Sang, T., Li, W., Li, L., Gao, Y., Qiu, W., & Zhou, H. (2020). A survey on perceptions of complementary and alternative medicine among undergraduates in China. Evidence-Based Complementary & Alternative Medicine: eCAM, 2020, 9091051. https://doi.org/10.1155/2020/9091051
Xue, C. C., Zhang, A. L., Lin, V., Da Costa, C., & Story, D. F. (2007). Complementary and alternative medicine use in Australia: A national population-based survey. Journal of Alternative & Complementary Medicine, 13(6), 643-650. https://doi.org/10.1089/acm.2006.6355
Yeo, A. S., Yeo, J. C., Yeo, C., Lee, C. H., Lim, L. F., & Lee, T. L. (2005). Perceptions of complementary and alternative medicine amongst medical students in Singapore – A survey. Acupuncture in Medicine, 23(1), 19-26. https://doi.org/10.1136/aim.23.1.19
Yildirim, Y., Parlar, S., Eyigor, S., Sertoz, O. O., Eyigor, C., Fadiloglu, C., & Uyar, M. (2010). An analysis of nursing and medical students’ attitudes towards and knowledge of complementary and alternative medicine (CAM). Journal of Clinical Nursing, 19(7-8), 1157-1166. https://doi.org/10.1111/j.1365-2702.2009.03188.x
Zollman, C., & Vickers, A. (1999). What is complementary medicine? British Journal of Medicine, 319(7211), 693-696. https://doi.org/10.1136/bmj.319.7211.693
*Justin Bilszta
Department of Medical Education,
Melbourne Medical School,
University of Melbourne, Australia
Parkville, Australia 3052
Tel: +61 3 8344 7826
Fax: +6567775702
Email: jbilszta@unimelb.edu.au
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









