Teleconferencing as a teaching modality for clinical year medical students: Lessons from COVID-19
Submitted: 18 October 2020
Accepted: 1 March 2021
Published online: 5 October, TAPS 2021, 6(4), 17-25
https://doi.org/10.29060/TAPS.2021-6-4/OA2418
Xin Rong Goh1, Chee Wai Ku2,4, Rajeswari Kathirvel1,2,4,5 & Kok Hian Tan1,3,4
1Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore; 2Department of Obstetrics and Gynaecology, KK Women’s & Children’s Hospital, Singapore; 3Department of Maternal Fetal Medicine, KK Women’s & Children’s Hospital, Singapore; 4Duke-NUS Medical School, Singapore; 5Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: Disease outbreaks (DO) result in unprecedented changes to the healthcare industry with far-reaching implications for medical education. The need to adapt to the fluidity during DO requires the delivery of the clinical medical curriculum to be flexible and effective. There is a lack of well-established guidelines on how medical education should be delivered during DO. This study aimed to explore the efficacy of teleconferencing-based platforms (TBP) as a teaching modality to overcome the challenges of clinical year medical education amidst a global pandemic and possibility of its use when there are no disease outbreaks (NDO).
Methods: A cross-sectional survey amongst 144 undergraduate clinical year students from a medical school in Singapore was conducted from May to June 2020, to explore their perspectives on TBP compared to physical venue-based platforms (PVBP). The survey consisted 5-point Likert scale and open-ended questions. Statistical and thematic analyses were performed.
Results: TBP provides greater convenience in travelling, note-taking and ability to overcome administrative challenges. Students strongly recommended its use in DO and NDO. However, students faced increased distractibility, decreased engagement and ease of raising questions, with a lower efficacy in content delivery. The above is dependent on the type of lessons delivered – clinical skills-based or didactic sessions.
Conclusion: TBP is a promising teaching modality for DO with promising possibility of extending its use to NDO. We propose a tri-faceted approach to target improvement in content delivery on TBP, mainly with measures to target propensity for decreased engagement and increased distractibility and to address the technology-related concerns.
Keywords: Medical Education, Teleconferencing, Teaching Modalities, Medical Students, COVID-19, Disease Outbreaks, Pandemics
Practice Highlights
- TBP was strongly recommended as substitute teaching modality during disease outbreaks.
- Students recommended TBP as a supplement for teaching even when there are no disease outbreaks.
- TBP enabled more convenience in travelling, note-taking and overcoming administrative challenges.
- Decreased engagement and increased distractibility noted when sessions are conducted on TBP.
- TBP can be improved via use of teaching aids and contextualising it to the lesson type.
I. INTRODUCTION
Singapore has experienced the escalation of its Disease Outbreak Response System Condition (DORSCON) status to ‘Orange’ due to COVID-19 outbreak on 7th February 2020. This has had significant implications in multiple sectors of the healthcare industry, including that of medical education (Samarasekera, Goh & Lau, 2020). It called for the rapid remodelling of the delivery of the medical education curriculum during a time when social containment and avoidance of large groups gatherings were enforced (Samarasekera & Gwee, 2021). In particular, to contain and prevent the spread of COVID-19, clinical rotations in healthcare institutions were temporarily suspended during the DORSCON Orange period (Chandratre, 2020; Samarasekera, Goh, Yeo et al., 2020).
Many institutions had since employed teleconferencing-based platforms (TBP) to deliver curriculum (Kanneganti et al., 2020; Srinivasan, 2020). TBP is defined as an avenue of e-learning that is ‘internet and local-networking based’ (Al-Shorbaji et al., 2015), enabling the provision of ‘synchronous’ (Dhir et al., 2017) real time audio-visual online interactions across different locations (Lamba, 2011). The literature exploring the use of TBP during DO is limited. Most studies on TBP focused on its use when there are no disease outbreaks (NDO). They described its facilitation of direct teacher-student engagement with quieter students (Fox, 2004) and raised its comparable effectiveness in fulfilling learning outcomes to traditional face-to-face lectures (Bertsch et al., 2007). TBP nonetheless faces deterrents to its implementation, including those of financial implications (Lim et al., 2009) and technical difficulties (Boatin et al., 2015; Lamba, 2011). During DO, it had helped to overcome concerns of social distancing and allowed the continuation of medical training (Kanneganti et al., 2020; Lim et al., 2009).
In spite of the above, it should be recognised that the temporary suspension of clinical rotations represent the absence of a cornerstone in delivery of the medical curriculum (Govindarajan et al., 2018; Jacobs & Samarasekera, 2012; Lim et al., 2009; Rawekar et al., 2016). This study thus chose to specifically focus on the clinical year students owing to the potential application of these findings to post-graduate clinical trainings. Furthermore, the different content and focus during the pre-clinical years (e.g. lack of clinical rotations, presence of anatomy and science practical) would likely raise concerns that are unique and non-generalisable to students in the clinical years. Pre-clinical students were therefor excluded from the current study.
While the use of TBP is largely commended (Fatani, 2020), it is pertinent to compare its efficacy to traditional physical venues-based platforms (PVBP) as a potential replacement or supplement for the delivery of the clinical curriculum during DO. This study aims to understand the ground-up perspective of clinical year students on TBP as an education tool during DO, as compared to PVBP. It also explored TBP’s suitability and effectiveness for the delivery of the undergraduate medical education when there are no disease outbreaks (NDO).
II. METHODS
A. Ethics Review
The following study was approved by NTU Institutional Review Board (IRB Reference number: 2020-05-003) with an exempt status.
B. Survey Design and Study Population
All undergraduate clinical year medical students from the Lee Kong Chian School of Medicine who had used teleconferencing as a part of their curriculum were invited to participate in an online survey via email and social-messaging platform that included an explanation of the study’s details. Informed consent was implied when the participant accessed the online survey administered via SurveyMonkeyÓ platform. Personal identifiers were not collected.
The cross-sectional survey consisted of a mix of 5-point Likert scale questions and open-ended questions. It was anticipated to be completed in 10 minutes. The questions were designed to evaluate their familiarity with teleconferencing and their opinions on teleconferencing as an educational tool as compared to physical venue-based sessions, e.g. traditional lectures, bedside and small group tutorials, and team-based learning. Their willingness to extend teleconferencing as a supplementary delivery tool for medical education in both DO and NDO situations were also explored.
The survey questions were developed de-novo with reference to the existing literature. The themes of platform accessibility and ease of raising questions were adapted from Al-Neklawy (2017) while that of engagement and distractibility were adapted from the Danielson’s Framework for Teaching – The classroom environment (Alvarez & Anderson-Ketchmark, 2011). The survey was then piloted amongst a group of medical students and faculty to assess content and face validity.
C. Statistical Analysis
Self-reported estimates on the number of prior use of teleconferencing were divided by 52 to determine weekly usage. Numerical values were awarded for the 5-point Likert scale as follows: Strongly agree (5), agree (4), neutral (3), disagree (2) and strongly disagree (1).
Paired 2 tailed T test was performed to determine the significance of difference in subjective efficacy of PVBP and TBP. To compare effect of gender on subjective efficacy for the two platforms and recommendations for TBP, independent T test and Fisher’s exact test were performed respectively. Pearson Correlation testing was performed to look for correlations between the variables. Kruskal-Wallis H test was used to study the effect of year of study on the responses. A p value of < 0.05 indicated statistical significance. Data analysis was performed using SPSSTM software (V.24.0).
D. Qualitative Analysis
Thematic analysis was performed for the elaborations and justifications provided by survey respondents. Concepts that were similar were used to guide the development of themes.
III. RESULTS
A. Sociodemographic Characteristics
A total of 144 out of 315 clinical year medical students completed the survey over a 3-week period from May to June 2020 (Year 3: n = 51; Year 4: n = 64; Year 5: n = 29). The survey response rate was 45.7%. Majority of students who responded were female (58.3%) and Year 4 (44.4%).
B. Teleconferencing Usage Patterns
Majority (73.6%) of students had used a teleconferencing platform, for educational and non-education purposes, in the past year prior to declaration of DORSCON Orange. The top three teleconferencing platforms by corrected mean weekly usage prior to DORSCON orange were Skype© (0.2), FaceTime© (0.2) and ZOOM© (0.1). During DOSRCON orange, the top three platforms for educational purposes by corrected mean weekly usage were ZOOM© (4.0), Skype© (0.3), Facetime© (0.1). (Table 1)
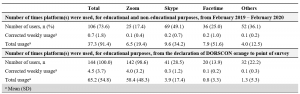
Table 1. Use of teleconferencing-based platforms by medical students
Corrected weekly usage was calculated as follows: (A) Total usage divided by 52, (B) Total usage divided by number of weeks from declaration of DOSRSCON orange to point of survey (For example: 1 week + 1 day would be considered as 2 weeks)
Others included: Whatsapp©, Microsoft Teams©, Google Hangouts©, WebEx©, Discord©, Houseparty©
C. Physical-Venue Based (PVBP) vs Teleconferencing-Based (TBP) Platforms
Students felt PVBP had significant engagement (mean = 4.0) and less distractibility (mean = 2.7). TBP had notable convenience (mean = 4.6), with negligible concerns on its safety (mean = 2.3) on a 5-point Likert scale. (Table 2)
When comparing TBP to PVBP, there was a significant increase in convenience (mean = 4.6 vs 3.8; p <0.001) with TBP. However, this was faced with increased distractibility (mean = 3.7 vs 2.7; p <0.001), decreased engagement (mean = 3.5 vs 4.0; p <0.001), ease of raising questions (mean: 3.4 vs 3.7; p =0.008) and efficacy in the delivery of content (mean: 4.0 vs 3.8; p =0.001). (Table 2)
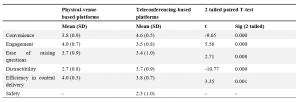
Table 2: Comparison of subjective efficacy of physical venue-based vs teleconferencing based platforms by clinical year medical students surveyed from May to June 2020 on a 5-point Likert Scale
Numerical values were assigned as follows: Strongly disagree (1), Disagree (2), Neutral (3), Agree (4), Strongly agree (5)
D. Correlations Between Responses
Based on Pearson’s correlation, students who were engaged on PVBP, tend to be more comfortable in raising questions (r = 0.301, p <0.001) and less distracted (r = -0.337, p <0.001) with PVBP. Similarly, students who felt engaged on TBP tend to feel comfortable in raising questions on TBP (r = 0.301, p <0.001), less distracted (r = – 0.353, p <0.001) and agree on its efficacy in content delivery (r = 0.570, p <0.001). Students who felt more distracted on PVBP tend to also be more distracted on TBP (r = 0.176, p <0.05). No significant correlations were found between prior teleconferencing experience on self-reported rating of PVBP and TBP.
Kruskal-Wallis H test showed a statistically significant difference in rating of convenience for TBP between different years of study (χ2 (2) = 18.1, p <0.001, mean (Year 3) 87.1, (Year 4) 69.8, (Year 5) 53.0). There were no statistically significant effects of gender on the responses.
E. Recommendations of Teleconferencing Platform
An overwhelming majority of students recommended use of TBP in DO (n = 143, 99.3%), 54.9% (n = 79) recommended it as a substitute, and 44.4% (n = 64) as a supplement for learning, whereas one student did not recommend it at all. A significant proportion continued to favour its use even during NDO (n = 121, 84.0%), although there was a slight shift in preference for it to be used as a supplement (Supplement: n = 108, 75%; Substitute: n = 13, 9.0%). (Table 3A)
There were no statistically significant effects of gender or year of study on the responses.
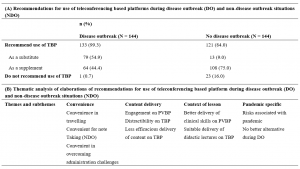
Table 3. Recommendations and suggested improvements for use of teleconferencing platforms during disease and non-disease outbreak situations by clinical year medical students surveyed from May to June 2020
N refers to the total number of elaborations provided for each type of recommendations, of which percentage (%) calculated reflects the percentage of respondents who raised a particular theme in their elaborations. n refers to the number of times the theme appeared per respondent.
Representative elaborations were quoted and tagged by the respondent’s demographic (Recommendation, Year of Study, Gender)
F. Qualitative Analysis
Thematic analyses revealed 10 main areas of discussion. These were categorised into three main themes that were common for both DO and NDO: convenience, content delivery and context of lesson (Table 3B). For the analysis for DO recommendations, a new theme materialised: Pandemic-specific considerations. Suggestions for improvements of TBP mainly fell into 3 categories – enhanced use of TBP teaching aids, ZOOM© fatigue and connectivity and technological concerns.
1) Convenience: Students indicated that TBP reduced their need to travel to teaching destinations, thereby saving on expenditure and time. This was especially useful when they were scheduled with a full day of lectures that did not require any clinical setting training, and during the exam period. For example, one student reported, “I value the time saved on travelling… more than the increased concentration and engagement of a face-to-face tutorial, given that exams are looming.” (Year 4, Female)
The ability to stream these sessions from home was advantageous as students could take additional measures to help sustain their attention, including the ease of taking refreshment breaks. Students valued the ease of taking notes as elaborated by one student as “easier to take screenshots of the slides so we don’t waste time copying the points.” (Year 5, Female)
Students noted TBP to be more convenient in arranging lectures across institutions. Specific to NDO, TBP was suggested as a potential mean to allow “teaching very large groups of people… combined stream classes” (Year 3, Male) and across medical schools. TBP also offered flexible scheduling arrangements. Examples included situations where participants are “feeling unwell but are worried about missing class” (Year 3, Female), “tutors with very busy or unpredictable schedules… which would require students to meet at odd or inconvenient timings” (Year 4, Male), hence minimising need for students to “stay back” (Year 5, Female) in the late evening.
2) Content delivery: Students discussed how triadic interactions between tutors and students, and amongst themselves were better afforded on PVBP. Nuances of social cues like facial expressions were cited as potentially beneficial for tutors to gauge students’ engagements. One student shared that “the tutor can gauge whether or not the content is appropriate based on the body language/facial expressions of the students which may be hard to do so on an online platform.” (Year 5, Female) Students also noted how TBP changed the nature of social interactions, making participants “less likely to speak up or participate… [with] the tutor [feeling] more distant.” (Year 4, Female)
The interactions between students as a reinforcement for learning surfaced as a crucial component. As one student shared, PVBP gave the “chance for the team to meet and learn from each other… quizzing each other, clarifying doubts, or sharing fun facts and important information [that]… cannot be done over teleconferencing.” (Year 3, Female)
Students reported that it was harder to stay focused during TBP sessions as one was in a “more comfortable location with no one monitoring your movements and actions” (Year 3, Male), unable to see the tutor in person and may have concomitant activities surrounding them. The implications of such distractibility were noted that TBP made it easier “to hide away and therefore not be present.” (Year 4, Female)
3) Context of lesson: Students felt their subjective assessment of TBP versus PVBP should factor in the type of lessons being delivered. It was unanimous that clinical-based teachings required use of PVBP to develop soft skills and appreciate clinical signs. To illustrate, one student shared, “medicine is an apprenticeship – there are many skills that cannot be learnt theoretically but must be observed in a clinical setting… Physical sessions are still very important to teach such skills, and should proceed with adequate safety measures in place. Otherwise, we will become doctors with good theoretical knowledge but poor practical/people skills” (Year 5, Female). However, many agreed that didactic lectures which involved pure unidirectional delivery of content could be suitably delivered over TBP as “lecturer… can still speak and present slides as usual.” (Year 3, Male)
4) Pandemic specific considerations: Students acknowledged the risk-benefit ratio of disease transmission and accommodation for the schedule of clinical tutors. One student summarised, “Additional benefits gained through physical venue-based outweighed by risks of disease transmission due to physical interaction.” (Year 3, Male) TBP was hence considered to be a safe and only suitable alternative to ensure continuity of curriculum delivery during DO.
5) Identified areas of improvement: Students raised suggestions to overcome the drawbacks of TBP in 3 main domains. Firstly, they recommended the enhanced used of teaching aids to increase engagement peer-peer interactions. Secondly, they raised the phenomenon of “ZOOM© fatigue” and the need to manage scheduling of tutorials. For example, one student shared, “People seem to think that online lectures are less mentally taxing since you’re at home, and proceed to pack the entire day full of lectures for couple weeks on end… there is no time to consolidate knowledge especially in the absence of opportunity to apply in a clinical setting.” (Year 4, Male) Hence, students suggested tutors to avoid “bombarding students with back-to-back tutorials, leading to information overload” (Year 4, Female) and decrease the maximum time per day to less than 4-5 hours. The inclusion of breaks between sessions as a mental break since tutors who are “swapping in… would not know if students are still engaged or fatigued.” (Year 4, Male)
Lastly, presence of poor connectivity contributed to streaming lags, with negative implications on students “concentration and ability to follow the lecture.” (Year 4, Female) The possibility of increasing tutors’ familiarity with the platform was cited to have facilitated a smoother conduct of lessons.
IV. DISCUSSION
A. Summary of Results
An overwhelming majority of students recommended the continued use of TBP during both DO and NDO. This is most likely due to the increased convenience in travelling, taking down notes, overcoming administrative challenges, and its suitable replacement for didactic lectures. The student’s perception of convenience of TBP correlated to the year of study, with the earlier clinical year students finding it more convenient than the final year students. Nevertheless, this should be evaluated against the background that end users range from enthusiastic ‘technophiles’ to ‘technophobes’, which influences the receptiveness towards e-learning platforms (Bruce, 1997; Fox, 2004).
Specifically during DO, it was viewed to be the best available alternative when considering the disease transmission risk and the busy schedules of the clinical tutors as they may have new responsibilities as front-liners in pandemics (Branch et al., 1997; Cook, 2006; Goh, 2020; Harden & Crosby, 2000; Ramani & Leinster, 2008).
The shift in preference of use of TBP as a substitute to supplement during NDO was noticeable. This can be due to many factors. There is a decreased engagement due to the reduced ability of tutors to assess nuances of social cues (Fox, 2004), greater distractibility and decreased ease of raising questions on TBP. Notably, peer-peer interaction is lost over TBP. Each student’s interaction is multidirectional: student with resource materials, with educator, and between students (Dhir et al., 2017). The value of such interactions and study groups in medical education should be duly taken into consideration (Burgess et al., 2014). Poorer engagement were further compounded by challenges with technology-related concerns and risks of “ZOOM© fatigue”.
Distractibility on TBP could be due to learning in a non-classroom environment (Fox, 2004) with a device that could also be used for non-educational purposes (Walsh, 2015). “ZOOM© fatigue” was likely due to lack of pre-fixed maximal time duration and the tendency for tutors to over-deliver and pile extra study materials (Fox, 2004) causing student’s to “feel tired and restless” (Srinivasan, 2020).
Interestingly, students’ innate personality and learning attitudes potentially influenced their perceptions of PVBP and TBP. Students who were more engaged on a platform, also felt more comfortable raising questions, were less distracted and believed that the platform was efficacious in delivering content. This demonstrates the difference between the “active and engaged learners” and the majority who are “silent lurkers (Fox, 2004). Similarly, students who felt more distracted on PVBP appeared to also be more distracted on TBP.
B. Recommendations
TBP as a teaching modality has an indisputable role during both DO and NDO. It is well-established that medical students experience significant psychological impact during DO (AlAteeq et al., 2020; Ullah & Amin, 2020), possibly related concerns on the impact of their studies (Lyons et al., 2020). Hence with the increased use of TBP, it is imperative that medical educators develop a deeper understanding on the potential short-comings of the platform and how best to maximise its utility as a teaching modality.
Nonetheless, it is vital to recognise that the efficacy of any new education tool depends on both educators and students. It would be better facilitated if the end user is familiar with the platform. It should be considered in light of its application and configuration (Cook, 2006) and ideally be managed and monitored by trained staff (Dhir et al., 2017; Harden, 2018). Moving forward, we recommend a tri-faceted approach to improve the content delivery of TBP during both DO and NDO (Figure 1).

Figure 1. Correlation of domains assessed for efficacy of teleconferencing-based platforms (TBP) with themes identified and suggestions to improve content delivery on TBP
1) Domain 1: Contextual use of TBP: Disease outbreak situations:
- Where physical appreciation of clinical skills through bedside tutorial or real-life clinical interactions might not be feasible, consider use of media and standardised patients to simulate clinical exposure.
- The supplemental use of standardised patients (Peters & Thrien, 2020) hones student’s clinical competence while facilitating the training of relevant skills needed for future practice (Khoo et al., 2020), a notable example in these evolving recent times also includes that of telemedicine (Williams & Song, 2016).
No disease outbreak situations
- TBP should mainly be used for didactic or team-based learning sessions, large group teaching sessions and for students who are unable to physically attend the lecture.
2) Domain 2: Targeting decreased engagement and increased distractibility:
- Use of multi-modal teaching aids, e.g. virtual quizzes, breakout rooms for small group engagement, drawing functions to better visually illustrate explanations.
- Monitoring of students’ current fatigue level in session via live polls at regular hourly intervals.
- Engagement of a central coordinator to regulate the maximum hours of online sessions per day, with considerations of suitable breaks between sessions.
- Prior assessment of student’s learning attitudes and class dynamics to enable tailored use of teaching aids.
3) Domain 3: Smoothening transition to TBP:
- Engagement of central coordinator to brief tutors on the functionality of TBP of choice to minimise technology unfamiliarity and maximise its utility in conducting sessions.
- Educational institutions to consider providing infrastructural support to students and educators, including dedicated spaces, electronic devices with internet connections, and easy access to technical support. These would help minimise network connectivity challenges and providing a conducive study environment for those who might face difficulties accessing TBP off-campus.
- Selective use of TBP as a supplement during NDO to increase both students and educator’s familiarity with the platform and as a learning tool, thereby enabling a smoother transition during DO.
C. Limitations
Our study has few limitations. We surveyed clinical year students from a single medical school and therefore, our study may not reflect the views of students from other medical schools with different teaching pedagogies and those of pre-clinical year students. Future studies should consider exploring the opinions of clinical tutors on PVBP and TBP and their perspective as educators in delivering such curriculum. In addition, given our limited sample size, some statistically significant sub-group patterns may not have been evident.
V. CONCLUSION
TBP is an important teaching modality during DO and NDO, especially with its increased convenience. However, it has certain issues including context-specific use, decreased engagement, increased distractibility and technological challenges. Our proposed potential interventions may help to maximise its utility and facilitate transition of its use in subsequent DO.
Notes on Contributors
Xin Rong Goh designed the study, recruited the participants, administered the survey, analysed the data and wrote the first and subsequent drafts of the manuscript. Rajeswari Kathirvel and Chee Wai Ku contributed to analysis of the data and writing of the manuscript. Kok Hian Tan contributed to the study design and reviewed the manuscript. All authors have read and approved the final manuscript.
Ethical Approval
The following study was approved by NTU Institutional Review Board (IRB Reference number: 2020-05-003) with an exempt status.
Data Availability
The ethical approval by NTU Institutional Review Board was based on the conditions that while the data is deidentified data, only study team members will have access to the raw data that will be stored on a password protected PC. The data could thus not be uploaded on a public data sharing platform.
Acknowledgement
The authors acknowledge Dr Joel Shi Quan Tan, Yong Loo Lin School of Medicine, National University of Singapore, for his contribution to the statistical analysis of the paper.
Funding
No funding sources was used for this research study.
Declaration of Interest
The authors have no conflicts of interest to declare.
References
AlAteeq, D. A., Aljhani, S., & AlEesa, D. (2020). Perceived stress among students in virtual classrooms during the COVID-19 outbreak in KSA. Journal of Taibah University Medical Sciences, 15(5), 398–403. https://doi.org/10.1016/j.jtumed.2020.07.004
Al-Neklawy, A. F. (2017). Online embryology teaching using learning management systems appears to be a successful additional learning tool among Egyptian medical students. Annals of Anatomy, 214, 9–14. https://doi.org/10.1016/j.aanat.2017.07.001
Al-Shorbaji, N., Atun, R., Car, J., Majeed, A., & Wheeler, E. (2015). eLearning health professional for undergraduate education. World Health Organistion. https://www.who.int/hrh/documents/14126-eLearningReport.pdf
Alvarez, M. E., & Anderson-Ketchmark, C. (2011). Danielson’s framework for teaching. Children and Schools, 33(1), 61–63. https://doi.org/10.1093/cs/33.1.61
Bertsch, T. F., Callas, P. W., Rubin, A., Caputo, M. P., & Ricci, M. A. (2007). Applied research: Effectiveness of lectures attended via interactive video conferencing versus in-person in preparing third-year internal medicine clerkship students for clinical practice examinations (CPX). Teaching and Learning in Medicine, 19(1), 4–8. https://doi.org/10.1080/10401330709336616
Boatin, A., Ngonzi, J., Bradford, L., Wylie, B., & Goodman, A. (2015). Teaching by teleconference: A model for distance medical education across two continents HHS public access. Open Journal of Obstetrics and Gynecology, 5(13), 754–761. https://doi.org/10.4236/ojog.2015.513106
Branch, W. T., Kroenke, K., & Levinson, W. (1997). The clinician-educator – Present and future roles. Journal of General Internal Medicine, 12(Suppl. 2), 1–4. https://doi.org/10.1046/j.1525-1497.12.s2.16.x
Bruce, B. C. (1997). Literacy technologies: What stance should we take? Journal of Literacy Research, 29(2), 289–309.
Burgess, A., McGregor, D., & Mellis, C. (2014). Medical students as peer tutors: A systematic review. BMC Medical Education, 14,115. https://doi.org/10.1186/1472-6920-14-115
Chandratre, S. (2020). Medical students and COVID-19: Challenges and supportive strategies. Journal of Medical Education and Curricular Development, 7. https://doi.org/10.1177/2382120520935059
Cook, D. A. (2006). Where are we with web-based learning in medical education? Medical Teacher, 28(7), 594–598. https://doi.org/10.1080/01421590601028854
Dhir, S. K., Verma, D., Batta, M., & Mishra, D. (2017). E-learning in medical education in India. Indian Pediatrics, 54(10), 871–877. https://doi.org/10.1007/s13312-017-1152-9
Fatani, T. H. (2020). Student satisfaction with videoconferencing teaching quality during the COVID-19 pandemic. BMC Medical Education, 20(1), 396. https://doi.org/10.1186/s12909-020-02310-2
Fox, R. (2004, December). SARS epidemic: Teachers’ experiences using ICTs. In R. Atkinson., C. McBeath., D. Jonas-Dwyer. & R. Phillips (Eds.), Beyond the comfort zone: Proceedings of the 21st Annual Conference of the Australasian Society for Computers in Learning in Tertiary Education (ASCILITE) (pp. 319-327). Australasian Society for Computers in Learning in Tertiary Education. http://www.ascilite.org.au/conferences/perth04/procs/fox.html
Goh, C. T. (2020, May 3). COVID-19: Guarding against burnout, compassion fatigue and trauma in frontline healthcare workers. Channel News Asia. https://www.channelnewsasia.com/news/singapore/covid-19-guarding-against-burnout-trauma-ttsh-ncid-frontline-12669280
Govindarajan, S., Vasanth, G., Kumar, P. A., Priyadarshini, C., Radhakrishnan, S. S., Kanagaraj, V., Balasubramanian, N., Kumar, P. N., Divya, T. J., & Aishwarya, C. N. (2018). Impact of a comprehensive early clinical exposure program for preclinical year medical students. Health Professions Education, 4(2), 133–138. https://doi.org/10.1016/j.hpe.2017.06.002
Harden, R. M. (2018). Medical teacher E-learning-caged bird or soaring eagle? Medical Teacher, 30(1), 1–4. https://doi.org/10.1080/01421590801938878
Harden, R. M., & Crosby, J. (2000). AMEE guide no 20: The good teacher is more than a lecturer – The twelve roles of the teacher. Medical Teacher, 22(4), 334–347. https://doi.org/10.1080/014215900409429
Jacobs, J. L., & Samarasekera, D. D. (2012). How we put into practice the principles of embedding medical students into healthcare teams. Medical Teacher, 34(12), 1008–1011. https://doi.org/10.3109/0142159X.2012.731097
Kanneganti, A., Sia, C.-H., Ashokka, B., & Ooi, S. B. S. (2020). Continuing medical education during a pandemic: An academic institution’s experience. Postgraduate Medical Journal, 96, 384- 386. https://doi.org/10.1136/postgradmedj-2020-137840
Khoo, S. A., Aswin, W., Shen, G. Q. Y., Haq, H. M., Junaidah, B., Yiew, J. L., Abiramy, M., & Sashikumar, G. (2020). Improving provider-patient communication skills among doctors and nurses in the children’s emergency department. The Asia Pacific Scholar, 5(3), 28–41. https://doi.org/10.29060/TAPS.2020-5-3/OA2160
Lim, E. C. H., Oh, V. M. S., Koh, D. R., & Seet, R. C. S. (2009). The challenges of “continuing medical education” in a pandemic era. Annals of the Academy of Medicine Singapore, 38(8), 724–726.
Lyons, Z., Wilcox, H., Leung, L., & Dearsley, O. (2020). COVID-19 and the mental well-being of Australian medical students: Impact, concerns and coping strategies used. Australasian Psychiatry, 28(6), 649–652. https://doi.org/10.1177/1039856220947945
Lamba, P. (2011). Teleconferencing in medical education: A useful tool. Australasian Medical Journal, 4(8), 442–447. https://doi.org/10.4066/AMJ.2011.823
Peters, T., & Thrien, C. (2020). The digital use of simulated patients in times of the corona pandemic – Considerations and proposals. GMS Journal for Medical Education, 37(7), Doc 93. https://doi.org/10.3205/zma001386
Ramani, S., & Leinster, S. (2008). AMEE guide no. 34: Teaching in the clinical environment. Medical Teacher, 30(4), 347–364. https://doi.org/10.1080/01421590802061613
Rawekar, A., Jagzape, A., Srivastava, T., & Gotarkar, S. (2016). Skill learning through early clinical exposure: An experience of Indian medical school. Journal of Clinical and Diagnostic Research, 10(1), JC01–JC04. https://doi.org/10.7860/JCDR/2016/17101.7022
Samarasekera, D. D., Goh, D. L. M., & Lau, T. C. (2020). Medical school approach to manage the current COVID-19 crisis. Academic Medicine, 95(8), 1126–1127. https://doi.org/10.1097/ACM.0000000000003425
Samarasekera, D. D., Goh, D. L. M., Yeo, S. P., Ngiam, N. S. P., Aw, M. M., Lim, M. M., Pillai, S., Lee, S. S., Mahadevan, M., Kow, A., Chong, Y. S., & Lau, T. C. (2020). Response and lessons learnt managing the covid-19 crisis by school of medicine, National University of Singapore. MedEdPublish, 9(1), 92, https://doi.org/10.15694/mep.2020.000092.1
Samarasekera, D. D., & Gwee, M. C. E. (2021). Adapting to change during challenging times. The Asia Pacific Scholar, 6(1), 1-2. https://doi.org/10.29060/TAPS.2021-6-1/EV6N1
Srinivasan, D. K. (2020). Medical students’ perceptions and an anatomy teacher’s personal crisis experience using an e-learning platform for tutorials during the Covid-19 crisis. Anatomical Sciences Education, 13(3), 318-319. https://doi.org/10.1002/ase.1970
Ullah, R., & Amin, S. (2020). The psychological impact of COVID-19 on medical students [Letter]. Psychiatry Research, 288, 113020. https://doi.org/10.1016/j.psychres.2020.113020
Walsh, K. (2015). Mobile learning in medical education: Review. Ethiopian Journal of Health Sciences, 25(4), 363–366. https://doi.org/10.4314/ejhs.v25i4.10
Williams, B., & Song, J. J. Y. (2016). Are simulated patients effective in facilitating development of clinical competence for healthcare students? A scoping review. Advances in Simulation (London, England), 1, 6. https://doi.org/10.1186/s41077-016-0006-1
*Goh Xin Rong
11 Mandalay Road,
Singapore 308232
Email: xinronggoh@yahoo.com.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









