Integration of medical device design training in clinical teaching – A case study
Submitted: 17 May 2020
Accepted: 2 September 2020
Published online: 4 May, TAPS 2021, 6(2), 91-93
https://doi.org/10.29060/TAPS.2021-6-2/CS2263
K. Anbarasi1 & Kasim Mohamed2
1Department of Dental Education, Sri Ramachandra Institute of Higher Education and Research, Chennai, India; 2Department of Maxillofacial Prosthodontics, Sri Ramachandra Institute of Higher Education and Research, Chennai, India
I. INTRODUCTION
Dental practitioners often encounter situations that require customising the prosthesis to satisfy the needs of patients. Artificial devices called dental appliances or prosthesis is custom fabricated for the functional, aesthetic, and psychological wellbeing of patients (Chu et al. 2013). The patient’s complaints may vary from missing natural teeth to extensive maxillofacial defects, and there is no single best rehabilitative therapy for these conditions. Designing our product is the choice, and this demands adaptive expertise, i.e., the ability to generate potential solutions (Mylopoulos et al. 2018). Maxillofacial Prosthodontics applies a variety of learning methods like systematic simulation laboratory exercises, See One, Do One, Teach One (SODOTO method), and supervised clinical practice to train the routine technical skills and clinical practice. To maximise the outcomes in the complex prosthetic treatment, the course specialists designed an “Interdisciplinary Device Development program (IDDP)”—a value-added course for the postgraduates in collaboration with the Biomedical Instrumentation Engineering Faculty of our Institution. IDDP is the first of its kind challenge-based learning model in Dentistry that uses innovations to deal with rehabilitation care beyond routine practice. This paper aims to present our IDDP model and programme outcomes.
II. METHODS
IDDP is structured in three stages referring to problem determination, design, and development. An abstract idea about the essential requirements and intellectual property protection is also included and is scheduled for 3 hours per week for 10 weeks’ (Table 1). The IDDP concept and curriculum were presented in the College Council meeting and subsequently in the Board of Studies and Academic Council. The proposal was approved and permitted implementation.
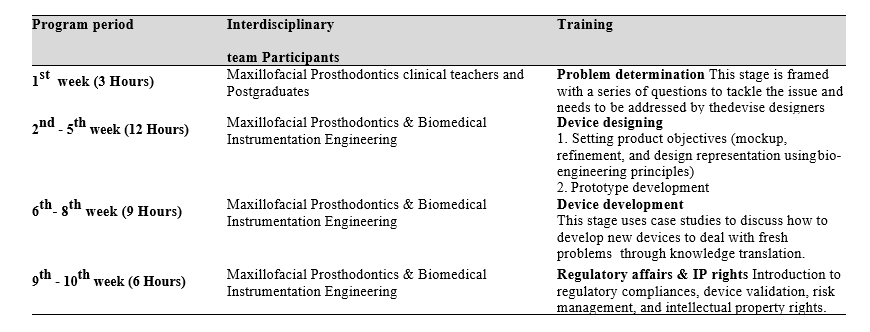
Table 1: IDDP curriculum framework
Participation in IDDP is mandatory for all postgraduates (PGs) of Maxillofacial Prosthodontics, but knowledge translation into practice is expected only when patients present with unique/challenging conditions. Chances of treating these patients are given for all PGs, but priority is given to those who showed valuable accomplishments in their regular clinical works. Once get allotted with such cases, the PG needs to work with their faculty in-charge, the primary consultant, a faculty member from biomedical engineering, and laboratory technicians.
The device designing demands advanced prosthodontic techniques and the attainment of competency depends on repeated practice. Skill assessment before accustoming it is not a safe practice hence the IDDP is not emphasising on assessments that reflect on summative grade, but performance assessment was made for the postgraduates who have undertaken the task to appraise their diligence, completeness, and problem-solving ability in a standard template, and supporting them to improve their learning.
III. INVENTIONS IN THE CLINICAL GROUNDS
A. Cheek Bumper
A Von Recklinghausen’s disease patient reported with a nodule on the left buccal mucosa and chewing difficulty. The patient expected non-surgical management, and there was a need for invention. Relieving the contact between the mucosal nodule and teeth was suggested as a solution and one PG student turned out the novel idea as an acrylic cheek bumper, an intraoral device that separated the growth 5mm away from the teeth surface. Wearing this appliance at mealtime solved the patient’s problem.
B. Training Pad for Jaw Reposition
A patient has undergone hemimandibulectomy on the right side. After a month, he reported aesthetic concern because of the deviation of the lower third of the face during jaw movements. Denture rehabilitation with a flange is a routine treatment to improve aesthetics. In our discussion, a PG student proposed to reposition the jaws before denture treatment to achieve the jaw compatibility for receiving the denture, hence optimising the success. The team accepted to transform the vision into reality. A prototype was prepared, and an intraoral acrylic pad with retainers was developed. Later the patient was treated with a prosthesis and he expressed his happiness in gaining back the chewing efficiency and confidence
C. Modified Impression Tray to Make Ear Prosthesis
To avoid the shape distortion and to get the adequate fine details in the replica, a postgraduate student in the existing tray pattern did a design modification and got an excellent result.
D. Compression Stent
A patient was referred for the management of a hypertrophic scar following ear piercing. The literature search revealed a solution of stent fabrication to cover the affected ear completely and wearing it full time for a year. The drawbacks like patient discomfort and long-time follow-up were highlighted and a PG student suggested redesigning the compression sent to cover only the scar region using claw type hair clip model. The patient was instructed to wear the stent for 10 to 12 hours per day. At the end of the fifth month, the scar was completely disappeared and she regained the ear lobe shape.
The devices in the process include:
- Mouth opening assisting device to treat trismus.
- Impression tray with size adjustable screws.
- Custom designed intraoral radio-productive device for patients receiving radiotherapy.
IV. STRENGTHS AND LIMITATIONS
A supportive curriculum always opens an avenue for innovation. Integration of Biomedical engineering solved the clinical problem by applying engineering principles, formulas, and materials in device designing as the dental specialty lacks the potential to practice the engineering domain. IDDP inspired our postgraduates to take part actively in treatment planning sessions. There is a positive shift in their clinical reasoning skill, describing the treatment options with their pros and cons, and finally specifying the target device by solving the limitations on the existing model or developing an alternative model.
The unresolved factors of IDDP include the struggle to tap the inventive potential of graduate students, their level of commitment, and time allocation. Formal assessment, patient satisfaction survey, student perception, and feedback should be considered.
V. MOVING FORWARD
Incorporating IDDP in the dental curriculum at the national level is the way forward.
VI. CONCLUSION
Our experience in IDDP evidences the innovation that happened on academic grounds. The structured training and opportunity to transform the learning into practice enhanced the confidence level of the clinicians to think out of the box, act as problem solvers, and shape the future health care industry.
Notes on Contributors
Dr. K. Anbarasi, MDS, PhD, devised the presented concept, framed the theoretical framework, wrote the manuscript, and agreed on its final form for submission.
Dr. Kasim Mohamed, MDS, involved in curriculum planning, conducted the programme, contributed to the final version of the manuscript, and agreed to its final form for submission.
Acknowledgment
The authors like to acknowledge the programme coordinators of IDDP.
Funding
The program was supported by the authors’ institution as an academic event.
Declaration of Interest
The authors have no conflict of interest.
References
Chu, K. Y., Yang, N. P., Chou, P., Chi, L. Y., & Chiu, H. J. (2013). Dental prosthetic treatment needs of inpatients with schizophrenia in Taiwan: A cross-sectional study. BMC Oral Health, 13(1), 8. https://doi.org/10.1186/1471-2458-10-482
Mylopoulos, M., Kulasegaram, K., & Woods, N. N. (2018). Developing the experts we need: Fostering adaptive expertise through education. Journal of Evaluation in Clinical Practice, 24(3), 674-677. https://doi.org/10.1111/medu.12893
*K. Anbarasi
Faculty of Dental Sciences,
Sri Ramachandra Institute of
Higher Education and Research,
Chennai, India.
Email: anbarasi815@gmail.com
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









