STarDom study – Applying systems theory framework for Internal Medicine senior residency career development in a Singapore ACGMEI Residency Programme
Published online: 2 May, TAPS 2018, 3(2), 6-18
DOI: https://doi.org/10.29060/TAPS.2018-3-2/OA1046
Joanne Kua, Mark Chan, Jolene See Su Chen, David Ng & Wee Shiong Lim
Department of Geriatric Medicine, Institute of Geriatrics and Active Ageing, Tan Tock Seng Hospital, Singapore
Abstract
Aims: Career counselling is a complex process. Traditional career counselling is unidirectional in approach and ignores the impact and interactions of other factors. The Systems Theory Framework (STF) is an emerging framework that illustrates the dynamic and complex nature of career development. Our study aims to i) explore factors affecting senior residency (SR) subspecialty choices, and ii) determine the suitable utility of the STF in career counselling.
Methods: A prospective observational cohort study of internal medicine residents was done. Surveys were collected at three time points. The Specialty Indecision Scale (SIS) assesses the individual components and expert consensus group derived the questions for the contextual components. We measured burnout using the Mashlach Burnout Inventory. Process influences were assessed via thematic analysis of open-ended question at the 3rd survey.
Results: 82 responses were collected. There was a trend towards older residents being ready to commit albeit not statistically significant. At year 1, overseas graduands (OR = 6.87, p= 0.02), lifestyle factors (t(29)=2.31, p=0.03, d= 0.91), individual factors of readiness (t(29) = -2.74, p=0.01, d= 1.08), indecisiveness (t(27)= -0.57, p=0.02, d= 0.99) and self- doubt (t(29)= -4.02, p=0.00, d= 1.54) predicted the resident’s ability to commit to SR. These factors change and being married (OR 4.49, p= 0.03) was the only factor by the 3rd survey. Male residents are more resolute in their choice (OR= 5.17, p= 0.02).
Conclusion: The resident’s choice of SR changes over time. The STF helps in understanding decision-making about subspecialty choices. Potential applications include: i) initiation of career counselling at year 1 and ii) reviewing unpopular SR subspecialties to increase their attractiveness.
Keywords: Internal Medicine Residents, Career Counselling, Senior Residency
Practice Highlights
- Career decision-making is a complex process and there is a need for a holistic approach to it.
- The Systems Theory Framework consists of a multifaceted range of content (individual and contextual factors) and process influences (change over time, recursiveness, chance) to illustrate the dynamic and complex nature of career development.
- The resident’s choice of senior residency changes over time throughout their residency. The factors that affect their subspecialty choice transit from individual factor of indecisiveness, self-doubt and readiness in year 1 to contextual factor of lifestyle by year 3.
- Male residents are more resolute in their choice of senior residency.
- Reasons for resident’s change of choice of senior residency include i) experience during rotation ii) lifestyle choices and iii) influences from peers and seniors.
I. INTRODUCTION
The choice of senior residency training is an important decision for internal medicine residents. There is a rich array of options ranging from sub-specializing in a chosen field among the many areas in internal medicine, through to continuing as a general internist. This is not an easy process and not surprisingly, there is great interest in examining the factors that influence this decision. Understanding what is important from the perspectives of residents will be helpful for ‘unpopular’ subspecialties as they seek to transform the subspecialty to become more attractive by incorporating factors that residents look for in their choice.
There has been extensive research in the field of career decision-making in medical professionals, with many emphasizing a plethora of factors and their organization (Osipow, 1999). Previous literature reported that 20% of physicians in residency training switched to unrelated specialties and 16% of physicians already in practice changed their specialty identification (Chase, Levine & Weisman, 1980; Holden & Levit, 1978). In recent years, controllable lifestyle factors like personal time for leisure, family and avocational pursuits, control of total weekly hours spent on professional responsibilities, and the presence of burnout have been cited as some of the main reasons for the ultimate choice of subspecialty (Chibnall, Enoch, & Schindler, 2013; Dorsey, Jarjoura, & Rutecki, 2003; Jackson, Nuthalapathy, & Owen, 2004). Other important factors include programme characteristics and the reputation and quality of the training programme (Aagaard, Dedier, & Julian, 2005; Redman, Saltman, & Straton, 1994). However, these studies were mostly done amongst Caucasian medical students and residents and there has hitherto been limited research exploring the relative importance of these factors in Asian societies and even fewer studies looking specifically at internal medicine residents and their subsequent choice of senior residency.
The landscape of Singapore’s postgraduate medical training programme has changed much since the transition to the residency system in 2010. Singapore is one of the first countries outside of the United States to partner with the Accreditation Council for Graduate Medical Education- International (ACGMEI) to introduce this training to our graduates (Huggan, Samarasekara, & Ooi, 2012; Samarasekara, Ooi, & Hooi, 2015). The first batch of residents graduated from junior residency in 2013 and there were anecdotal accounts of “surprises” in choice of senior residency programme, namely those who made decisions that were contrary to prior indicated choices at the start of residency training. While the exact reasons are unclear, some have attributed this observed trend to the younger age at which trainees in Singapore enter residency training. Because medical education in Singapore’s largest medical school is an undergraduate course, residents in Singapore are therefore of a younger age (around 25 years of age) when choosing senior residency fellowship compared to their counterparts in the United States (more than 28 years of age). Thus, the relative ability to decide on their senior residency training and to commit to it upon completion of their residency training may be less firmly established.
Against this background, career counselling assumes salience in helping trainees navigate their career choices. Career counselling comprises both the principles of career theory and counselling theory. Traditional career theory used to focus on specific factors at a definite time point which are relevant to career choice, ignoring the possibility of other factors and the interactions that determine the subsequent career choice. Traditional career counselling is also seen only as a problem solving process where one’s knowledge of self is matched to the knowledge about the world of work, neglecting other important elements like ability, personality and/or aptitude. These have been perceived as being too narrow as it did not encompass other elements of the social or the environmental-societal systems in the process of career decision making (Chen, 2003). This has resulted in the recent emphasis of career counselling on the holistic approach to an individual and also on the effect that multimodal interactions of various elements have on eventual career choice (Patton & McMahon, 2014).
The Systems Theory Framework (STF) (McMahon, & Patton, 1999) (Figure 1) is an emerging framework in career counselling. It is a metatheoretical framework consisting of a multifaceted range of content and process influences to illustrate the dynamic and complex nature of career development. It accommodates not just the traditional perspectives of identifying what works best for the individual but also include a more holistic approach of incorporating many other elements into the decision making process itself. Content influences comprise the interconnecting systems of individual, social and environmental-societal factors (the latter two collectively classified as contextual) while process influences are made up of recursiveness (i.e. interaction between influences), change over time, and chance. Another strength of the STF is that it provides the user with a link between theory and practice, thus bridging the gap inherent in the more theory-centric traditional approaches (McMahon & Patton, 1999). The practical application of STF for guiding career assessment (Kontosh, & Zimmerman, 2007) and counselling (Patton & McMahon, 2006) have been previously described but its utility for understanding career choices in the context of internal medicine senior residency has not been well studied.
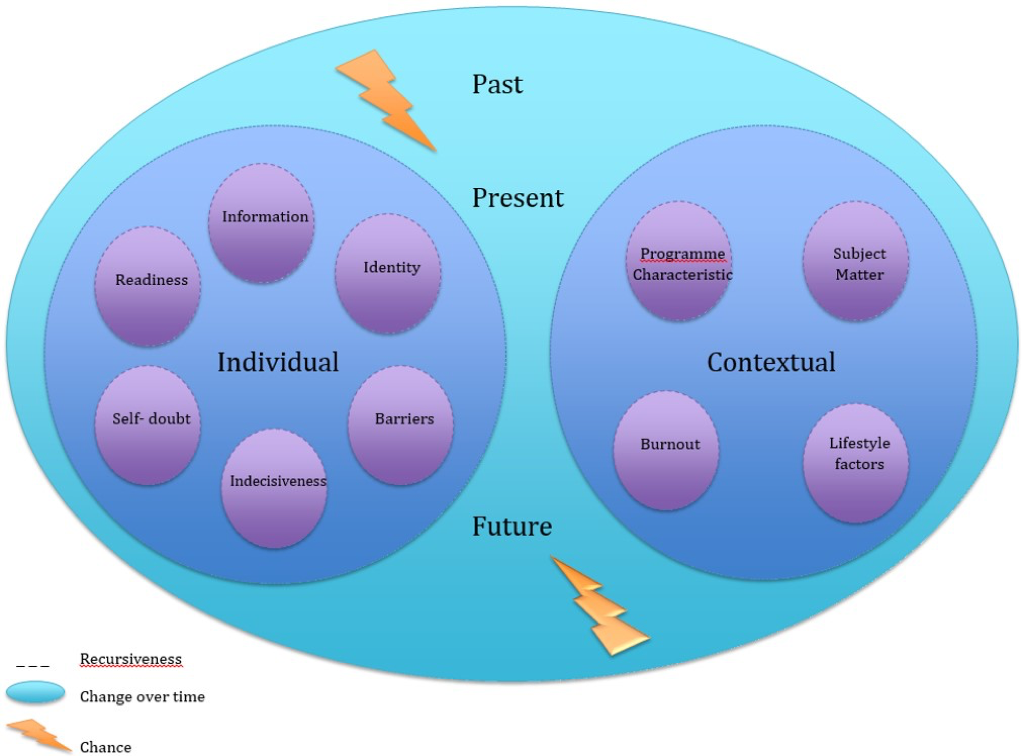 Figure 1. The Systems Theory Framework (STF)
Figure 1. The Systems Theory Framework (STF)
Therefore, using the lenses of the STF, our study aims to evaluate factors that affect the choice of senior residency amongst internal medicine residents and to understand the utility of the STF as a potential framework for career decision-making in this context.
II. METHODS
This is an observational cohort study of all the year 1 internal medicine residents entering the National Healthcare Group-Alexandra Health Private Limited (NHG-AHPL) residency programme in 2013. The Internal medicine residency programme in Singapore consists of 3 years of junior residency followed by 3 years of senior residency. Options for senior residency range from general internal medicine, to procedural subspecialties such as cardiology and non-procedural subspecialties such as endocrinology. There are no exclusion criteria. These residents are followed up for 3 years through their junior residency. Anonymity was maintained for all responses. We collected a total of 82 responses over 3 years.
A. Survey
We collected baseline demographics including age, sex, socioeconomic status, location of medical school, marital status at time of choice and number of years post-graduation. We also collected information pertaining to the individual and contextual systems of the STF as well as the choice of their subspecialty. The surveys were administered at three time points: beginning of year 1, beginning of year 2 and end of year 2. We chose to do the third survey at the end of year 2 because we wanted to survey residents before they officially indicate their choice of senior residency at the beginning of year 3. Surveys were done for the entire month to ensure that we capture as many responses as possible.
B. Systems Theory Framework (STF)
The STF explores individual as well as contextual factors which affect one’s choice of career. The individual system is central to the STF, and describes a range of personal influences that can affect career development such as age, beliefs, personality, values and ability. In contrast, contextual factors examine the influence of the social and environmental-societal systems.
To study the individual factors, we adapted the 35-item Specialty Indecision Scale (SIS) (Alexander, Osipow, & Savickas, 1985; Early, Richard, & Savickas, 2007) that looks at 6 major career concerns: readiness, information, identity, barriers, indecisiveness and self-doubt. Readiness assesses whether the resident is ready to make a decision. Information refers to the need for the resident to locate sources of information and guidance to find out more before he can make a career decision. Identity addresses the need to find out more about themselves before exploring suitable specialties. Barriers refer to external conflicts (related to the specialties or persons) that prevent the resident from making a choice. Indecisiveness identifies internal conflicts that prevent the resident from choosing. Self-doubt refers to psychosocial factors like self-confidence or anxiety that prevents decision-making.
Each item is scored on a 4-point Likert scale ranging from 1 (Not at all like me) to 4 (Exactly like me). The mean scale score and scale standard deviation for each cohort are calculated, from which the SIS standard score is then derived using the pre-determined formula: SIS Standard score= 50 + ((Raw Scale Score- Mean Scale Score)/ Scale Standard Deviation) x 10. Scores are considered low if less than 40, moderate if between 40-60 and high if >60. A high score reflects an area of concern that should be addressed during subsequent career counselling.
To study the contextual system, we included factors like programme characteristics, lifestyle, subject matter, and the presence of burnout. The questions in each component are derived through expert group consensus after extensive review of the literature and team discussion. Responses are scored on a 5-point Likert scale ranging from 1 (strongly agree) to 5 (strongly disagree). We measured the degree of burnout in our residents using the Maslach-Burnout Inventory-Human Services Survey (MBI) (Jackson, Leiter & Maslach, 1996). The MBI is a 22-item self-administered questionnaire that assesses the three components of the burnout syndrome, namely emotional exhaustion, depersonalization and reduced personal accomplishment. It has been extensively used amongst healthcare professionals and demonstrates good reliability and validity different cultural settings (Chou, Hecker, & Martin, 2012; Endler, Fuchs, & Messenholl-Strehler, 2011; Endler, Fischer, & Mitsche, 2013; Gillespie, Kalliath, & O’Driscoll, 2000). Responses are collected on a 7-point Likert scale where 0 reflects a statement that the resident has never felt and 6 a statement that the resident feels every day. For the assessment of processes influences, we collected responses at the third time point as to whether there has been a change in their subspecialty choice and the reasons for the change. The respective scales chosen have been based on prior validation and relevance.
C. Outcome Measure
Primary outcome was their readiness to commit to an area of specialization for senior residency training like geriatric medicine, cardiology etc at each time the survey was done.
D. Statistical Analyses
All statistical analyses were performed using SPSS version 21.0. We performed Chi square test to compare dichotomous variables between groups and the student t-test for unpaired data to compare parametric continuous data. The level of significance was taken to be 5%.
For each of the 3 time-points, we compared demographics, individual factors (SIS scores) and contextual factors between respondents who were ready to commit with those who were not. We performed subgroup analysis comparing the group whose choice of senior residency changed with those whose choice remained constant. For the former group, we also performed thematic analysis of open-ended responses to ascertain the reasons for change.
III. RESULTS
We collected a total of 82 responses over the 3 time points from July 2013 to June 2015. The number of respondents was respectively 31 (64.6% of eligible residents), 30 (62.5%), and 21 (43.8%) for the three surveys (Table 1).
A. Beginning of Year 1
Respondents had a mean age of 26.13 ± 2.33 (23-31) years. There was slightly more females in this cohort (54.8%) and majority of them were single (93.5%) and graduated from local universities (67.7%).
Amongst this cohort, there were 9 who were ready to commit and 22 who weren’t ready to commit (Table 2a). On univariate analyses, those who studied overseas (OR= 6.87, p= 0.02) tended to be more ready to commit than those who studied locally. Looking at the various components of the SIS score, the career concerns of readiness (t(29)= -2.74, p=0.01, d= 1.08), indecisiveness (t(27)= -0.57, p=0.02, d= 0.99) and self-doubt (t(29)= -4.02, p=0.00, d= 1.54) were significantly higher in the group who wasn’t ready to commit. Lifestyle factors seem to play an important role in the choice of senior residency for those who are ready to commit at year 1 (t(29) = 2.31, p=0.03, d= 0.91). There was also a trend towards those who are ready to commit being older (27.11 ± 2.03 years compared to 25.73 ± 2.37, t(29) = 1.53, p=0.14, d=0.60).
| Variables | Year 1 (n=31) | Year 2 (n=30) | Year 3 (n=21) |
| Baseline demographics | |||
| Age (Mean ± SD)
Gender (n, %) Male Female Marital Status (n, %) Single Married University (n, %) Local Overseas PGYa (n, %) 1-3 years >3 years |
26.13 ± 2.33
(23-31)
14 (45.2%) 17 (54.8%)
29 (93.5%) 2 (6.5%)
21 (67.7%) 10 (32.3%)
22 (71.0%) 9 (29.0%) |
25.93 ± 1.66
(24-30)
13 (43.3%) 17 (56.7%)
28 (93.3%) 2 (6.7%)
23 (76.7%) 7 (23.3%)
23 (76.7%) 5 (16.7%) |
27.48 ± 2.02
(25-33)
6 (28.6%) 15 (71.4%)
17 (81.0%) 4 (19.0%)
12 (57.1%) 9 (42.9%)
14 (66.7%) 7 (33.3%) |
| Individual Factors | |||
| Specialty Indecision Scale (SIS) (Mean ± SD)
Readiness
Information
Identity
Barriers
Indecisiveness
Self-doubt
Other concerns
Readiness category (n, %) Low Moderate High Information category (n, %) Low Moderate High Identity category (n, %) Low Moderate High Barriers category (n, %) Low Moderate High Indecisiveness category (n, %) Low Moderate High Self-doubt category (n, %) Low Moderate High |
49.99 ± 10.01 (30.40- 67.21) 49.98 ± 13.96 (29.25- 72.90) 50.00 ± 10.00 (31.44- 69.90) 49.99 ± 9.99 (34.86- 76.01) 50.01 ± 10.01 (31.74- 63.82) 50.00 ± 9.99 (27.28- 67.86) 49.98 ± 9.98 (27.83- 67.83)
6 (19.4%) 21 (67.7%) 4 (12.9%)
8 (25.8%) 14 (45.2%) 9 (29.0%)
5 (16.1%) 17 (54.8%) 9 (29.0%)
6 (19.4%) 22 (71.0%) 3 (9.7%)
7 (22.6%) 18 (58.1%) 6 (19.4%)
6 (19.4%) 22 (71.0%) 3 (9.7%) |
50.00 ± 9.69 (24.34- 64.34) 50.00 ± 10.00 (31.91- 68.09) 49.98 ± 10.01 (27.64- 70.27) 50.00 ± 10.01 (38.05- 77.88) 49.99 ± 9.99 (23.82- 64.78) 49.99 ± 10.01 (28.91- 68.64) 50.01 ± 10.01 (23.00- 62.53)
6 (20.0%) 17 (56.7%) 7 (23.3%)
6 (20.0%) 20 (66.7%) 4 (13.3%)
6 (20.0%) 20 (66.7%) 4 (13.3%)
4 (13.3%) 23 (76.7%) 3 (10.0%)
3 (10.0%) 20 (66.7%) 7 (23.3%)
4 (13.3%) 21 (70.0%) 5 (16.7%) |
50.02 ± 10.00 (29.16- 69.31) 50.00 ± 10.01 (33.37- 68.62) 49.99 ± 10.01 (30.61- 69.89) 50.00 ± 9.97 (29.26- 73.81) 50.00 ± 9.99 (29.44- 69.81) 50.01 ± 10.01 (30.96- 69.32) 50.00 ± 9.98 (28.15- 67.76)
2 (9.5%) 17 (81.0%) 2 (9.5%)
4 (19.0%) 14 (66.7%) 3 (14.3%)
2 (9.5%) 17 (81.0%) 2 (9.5%)
4 (19.0%) 16 (76.2%) 1 (4.8%)
3 (14.3%) 14 (66.7%) 4 (19.0%)
3 (14.3%) 15 (71.4%) 3 (14.3%) |
| Contextual Factors | |||
| Programme characteristics
(Mean ± SD) Subject matter (Mean ± SD) Lifestyle Factors (Mean ± SD) Burnoutb (n, %) No |
12.10 ± 2.22
(8-16) 8.81 ± 2.63 (5-18) 7.55 ± 2.03 (3-12)
27 (87.1%) |
12.30 ± 2.52
(6-17) 7.70 ± 1.69 (4-11) 6.87 ± 2.18 (3-12)
25 (83.3%) |
12.00 ± 2.57
(7-17) 8.00 ± 1.76 (5-12) 7.71 ± 2.72 (4-15)
19 (90.5%) |
| Yes | 4 (12.9%) | 4 (13.3%) | 2 (9.5%) |
| Readiness to commit (n, %)
Yes No |
9 (29%) 22 (71%) |
10 (33.3%) 20 (66.7%) |
11 (52.4%) 9 (42.9%) |
aPost graduate year
bMeasured by Mashlach Burnout Inventory (Human Services Survey
Table 1. Characteristics of the respondents over the 3 surveys
| Variables | Those who are ready to commit
(n=9) |
Those who are not ready to commit (n= 22) | Odds Ratio | P-value |
| Baseline demographics | ||||
| Age (Mean ± SD)
Gender (n, %) Male Female Marital Status (n, %) Single Married University (n, %) Local |
27.11 ± 2.03
(24-30)
4 (44.4%) 5 (55.6%)
8 (88.9%) 1 (11.1%)
3 (33.3%) |
25.73 ± 2.37
(23-31)
10 (45.5%) 12 (54.5%)
21 (95.5%) 1 (4.5%)
18 (81.8%) |
0.00
0.46
6.87 |
0.14
0.96
0.50
0.02c |
| Overseas
PGYa (n, %) 1-3 years >3 years Housing (n, %) HDB Condominium Landed Property |
6 (66.7%)
6 (66.7%) 3 (33.3%)
5 (55.6%) 1 (11.1%) 3 (33.3%) |
4 (18.2%)
16 (72.7%) 6 (27.3%)
7 (31.8%) 4 (18.2%) 11 (50%) |
0.11
2.86 2.62 |
0.74
0.41 0.27 |
| Individual Factors | ||||
| Standard Score SIS
(Mean ± SD) Readiness
Information
Identity
Barriers
Indecisiveness
Self-doubt
|
43.01 ± 10.45 (30.40- 58.01) 43.35 ± 13.76 (29.25- 64.96) 48.27 ± 9.65 (37.85- 60.29) 49.49 ± 8.76 (34.86- 59.55) 43.62 ± 10.62 (31.74- 61.15) 40.80 ± 9.72 (27.28- 56.26) |
52.84 ± 8.49 (30.40- 67.21) 52.69 ± 13.41 (29.25- 72.90) 50.67 ± 10.29 (31.44- 69.90) 50.19 ± 10.64 (34.86- 76.01) 52.75 ± 8.59 (34.41- 63.82) 53.44 ± 7.52 (41.17- 67.83)
|
0.01c
0.09
0.57
0.86
0.02c
0.00c |
|
| Contextual Factors | ||||
| Programme characteristics
(Mean ± SD) Subject matter (Mean ± SD) Lifestyle factors (Mean ± SD) Burnoutb (n, %) No Yes |
11.89 ± 2.67
(8-16) 8.78 ± 2.11 (6-12) 8.78 ± 2.59 (3-12)
8 (88.9%) 1 (11.1%) |
12.19 ± 2.06
(8-15) 8.82 ± 2.86 (5-18) 7.05 ± 1.56 (3-10)
19 (86.4%) 3 (13.6%) |
0.04 |
0.74
0.97
0.03c
0.85 |
aPost graduate year
bMeasured by Mashlach Burnout Inventory (Human Services Survey)
c P< 0.05
Table 2a. Survey at beginning of year 1
B. Beginning of Year 2
The mean age of respondents was 25.93 ± 1.66 (24-30) years. There was slightly more females (56.7%) and most were still single (93.3%). Compared to the first survey, there were more local graduates (76.7%) and most of them were within one to three years post-graduation from medical school (76.7%).
There were 10 (33.3%) residents who were ready to commit and 20 (66.7%) not ready to commit. There was a non-significant trend towards those who are ready to commit being older (26.70 ± 2.00 years compared to 25.55 ± 1.36 years, t(13.3) = 1.64, p=0.13, d= 0.72). The component of readiness in SIS was significantly higher for those who weren’t ready to commit (t(28) = -2.89, p=0.01, d= 1.12). Programme characteristic was also considered to be important for the group that was ready to commit even though not statistically significant (t(28) = 1.93, p=0.06, d= 0.75).
C. End of Year 2
Respondents had a mean age of 27.48 ± 2.02 (25-33) years. Most were females (71.4%) and the proportion of married residents increased from the previous 2 surveys to 19%. There were also more overseas graduates who responded for this interview (42.9%) and around one third of them are more than 3 years post-graduation from medical school (33.3%).
Eleven (52.4%) residents were ready to commit compared to 10 residents who were not (Table 2b). Interestingly, those who were married tended to be more ready to commit compared to those who are still single (OR= 4.49, p=0.03). Males also tended to be more ready to commit compared to females but this trend was not statistically significant (OR= 3.23, p=0.07). There was a non-statistically significant trend towards lifestyle factor being more important to those who are ready to commit (t(19) = 1.90, p=0.07, d= 0.84).
| Variables
|
Those who are ready to commit
(n=11) |
Those who are not ready to commit (n= 10) | Odds Ratio | p-value |
| Baseline demographics | ||||
| Age (Mean ± SD)
Gender (n, %) Male Female Marital Status (n, %) Single Married University (n, %) Local Overseas PGYa (n, %) 1-3 years >3 years Housing (n, %) HDB Condominum Landed Property |
28.09 ± 2.47
(25-33)
5 (45.5%) 6 (54.5%)
7 (63.6%) 4 (36.4%)
5 (45.5%) 6 (54.5%)
6 (54.5%) 5 (45.5%)
4 (36.4%) 4 (36.4%) 3 (27.3%) |
26.80 ± 1.14
(26-29)
1 (10.0%) 9 (90.0%)
10 (100.0%) 0 (0.0%)
7 (70.0%) 3 (30.0%)
8 (80.0%) 2 (20.0%)
4 (40.0%) 1 (10.0%) 5 (50.0%) |
3.23
4.49
1.29
1.53
0.25 1.67 |
0.14
0.07
0.03c
0.26
0.22
0.30 0.62 |
| Individual Factors | ||||
| Standard Score SIS
(Mean ± SD) Readiness
Information
Identity
Barriers
Indecisiveness
Self-doubt
|
48.07 ± 10.30 (29.16- 58.36) 50.27 ± 10.74 (33.37- 65.42) 49.44 ± 10.61 (30.61- 66.32) 48.16 ± 9.60 (29.26- 58.96) 49.07 ± 10.49 (29.44- 69.81) 49.39 ± 12.62 (30.96- 69.32) |
52.15 ± 9.74 (40.11-69.31) 49.72 ± 9.73 (36.57- 68.62) 50.61- 9.85 (37.75-69.89) 52.03 ± 10.49 (39.16- 73.81) 52.11 ± 9.49 (38.76- 66.71) 50.68 ± 6.69 (41.92- 61.10) |
0.36
0.90
0.80
0.39
0.37
0.78 |
|
| Contextual Factors | ||||
| Programme characteristics
(Mean ± SD) Subject matter (Mean ± SD) Lifestyle factors (Mean ± SD) Burnoutb (n, %) No Yes |
12.18 ± 2.71
(8-17) 8.45 ± 1.92 (5-12) 8.73 ± 3.04 (4-15)
11 (100%) 0 |
11.80 ± 2.53
(7-16) 7.50 ± 1.51 (5-10) 6.60 ± 1.90 (4-9)
8 (80.0%) 2 (20.0%)
|
2.43 |
0.74
0.22
0.07
0.12 |
| Has SRd choice changed? (n, %)
No Yes |
8 (72.7%) 3 (27.3%) |
5 (50%) 5 (50%) |
1.15 |
0.29 |
aPost graduate year
bMeasured by Mashlach Burnout Inventory (Human Services Survey)
c P< 0.05
d Senior residency
Table 2b. Survey at end of year 2
For the last survey, we also asked the residents whether their choice of senior residency has changed from when they were in first year of residency and out of those who were ready to commit, 72.7% were steadfast in their choice. However, for those who were not ready to commit, 50% had changed their choice since first year of residency.
D. Change of choice of Senior Residency (SR)
Eight residents had a change of SR choice whereas 13 (61.9%) did not (Table 3). The mean age for the latter group was slightly higher (27.77 ± 2.39 years compared to 27.00 ± 1.20 years, t(19) = -0.84 p= 0.41, d=0.38). The only significant finding was that male residents appear to be more resolute in their choices and tended not to change them (OR= 5.17, p= 0.02).
| Variables
|
Those whose SRd choice changed (n=8) | Those whose SRd choice didn’t change (n=13) | Odds Ratio | P-value |
| Baseline demographics | ||||
| Age (Mean ± SD)
Gender (n, %) Male Female Marital Status (n, %) Single Married University (n, %) Local Overseas PGYa (n, %) 1-3 years >3 years Housing (n, %) HDB Condominium Landed Property |
27.00 ± 1.20
(26-29)
0 (0%) 8 (100%)
6 (75.0%) 2 (25.0%)
6 (75.0%) 2 (25.0%)
5 (62.5%) 3 (37.5%)
4 (50.0%) 2 (25.0%) 2 (25.0%) |
27.77 ± 2.39
(25-33)
6 (46.2%) 7 (53.8%)
11 (84.6%) 2 (15.4%)
6 (46.2%) 7 (53.8%)
9 (69.2%) 4 (30.8%)
4 (30.8%) 3 (23.1%) 6 (46.2%) |
5.17
0.30
1.68
0.10
0.67 0.33 |
0.41
0.02c
0.59
0.20
0.75
0.73 0.31 |
| Individual Factors | ||||
| Specialty Indecision Scale (SIS)
(Mean ± SD) Readiness
Information
Identity
Barriers
Indecisiveness
Self-doubt |
49.23 ± 11.87 (32.81- 69.31) 50.99 ± 11.10 (36.57- 68.62) 47.13 ± 10.27 (37.75- 69.89) 50.92 ± 11.21 (39.16- 73.81) 51.18 ± 10.23 (38.76- 66.71) 50.48 ± 9.43 (39.18- 66.58) |
50.50 ± 9.17 (29.16- 50.50) 49.39 ± 9.70 (33.37- 65.42) 51.76 ± 9.83 (30.61- 66.32) 49.44 ± 9.58 (29.26- 58.96) 49.27 ± 10.19 (29.44- 69.81) 49.72 ± 10.72 (30.96- 69.32) |
0.79
0.73
0.32
0.75
0.68
0.87 |
|
| Contextual Factors | ||||
| Programme characteristics
(Mean ± SD)
Subject matter (Mean ± SD)
Lifestyle factors (Mean ± SD) Burnoutb (n, %) No Yes |
12.00 ± 2.98
(7-16)
7.88 ± 1.73 (5-10)
6.88 ± 1.64 (4-9)
7 (87.5%) 1 (12.5%) |
12.00 ± 2.42
(8-17)
8.08 ± 1.85 (5-12)
8.23 ± 3.17 (4-15)
12 (92.3%) 1 (7.7%) |
0.13 |
1.00
0.81
0.28
0.72 |
aPost graduate year
bMeasured by Mashlach Burnout Inventory (Human Services Survey)
c P< 0.05
d Senior residency
Table 3. Comparison of those whose choice of senior residency changed
Analysis of the open-ended responses to reasons for the change in SR revealed 3 main themes: 1) experience and exposure during the rotation, 2) lifestyle choices and life events that altered priorities, and 3) influences from peers and seniors that led to the change in their choice of SR. Rotations through the different postings allowed the residents the opportunity to experience subspecialties they previously had no rotation through as a student. Residents also were able to work with the different consultants within the department who impacted them sufficiently to make them want to join the department. Many residents quoted lifestyle factors as an important consideration, with priorities changing as they progressed through residency and the corresponding seasons in their life. Lastly, interactions with peers who had done the rotation or speaking to seniors who had chosen the subspecialty helped to shape residents’ understanding of the subspecialty and what it actually entailed.
IV. DISCUSSION
Our study contributes to the body of evidence by using the STF to longitudinally examine factors that affect the choice of senior residency programme among internal medicine residents. Our study shows that factors affecting a resident’s subspecialty choice were dynamic and differed throughout the course of their training. For first year residents, individual factors among those who are not ready to commit and lifestyle factors were important determinants in the first year. However, these factors changed in the subsequent 2 surveys such that by the 3rd survey, only being married appear to influence the resident’s readiness to commit with life-style factors re-emerging as an important factor. The process influences highlighted in the STF are also evident by the recursiveness and dynamic nature over time of career choices, such that residents’ senior residency decisions are influenced by their experience and exposure during the rotation interacting with lifestyle choices or life events, and influences from peers and seniors.
In our study, first year residents who are transitioning into their training are especially vulnerable and struggle more with self-doubt, indecisiveness and readiness components of the SIS. This suggests that the SIS may be a useful tool to delineate individual factors of the STF for career counselling among junior residents. In support of this, other studies have reported that the SIS is a reliable tool with good internal consistency and relates well with subsequent specialty choice (Kantosh, & Zimmerman, 2007). Contrary to other studies where burn-out appears to be a prime motivational factor for the choice of certain subspecialties (Chibnall, Enoch, & Schindler, 2013), our study shows that the presence of burnout did not affect the readiness for the residents to commit to a choice of senior residency. In contrast to earlier studies from the West (Chibnall, Enoch, & Schindler, 2013; Dorsey, Jarjourna, & Rutecki, 2003; Holden, & Levit, 1978; Jackson, Nuthalapaty & Owen, 2004; Redman, Saltman, & Straton, 1994), there is a trend towards older residents being more ready to commit to their SR choice, suggesting that age may be a salient factor in our system where trainees are younger compared to their America’s counterparts.
Taken together, our results support the recent shift in career (subspecialty) counselling away from a once-off objective cognitive problem-solving process, towards a developmental process where the mentor/counsellor interacts to discover the resident’s work personality, define the work competencies, identify information deficits, as well as recognize anxieties and help deal with emotions that may confound the career decision making (Herr, 1997). In this regard, the STF provides a useful over-arching framework to guide subspecialty career counselling in the current era of residency-based training where internal medicine residents enter training at a younger age. It provides a comprehensive framework that incorporates the influence of individual (readiness, identity, barriers, indecisiveness, information and self-doubt) and contextual (programme characteristics, subject matter and lifestyle) factors on career decision-making. By recognizing the recursiveness of these factors with internal and external influences over time, the STF also helps facilitate this circular feedback loop in the longitudinal discussions with residents by allowing constant interaction and review of how their choice of senior residency may change during course of residency training.
Our study had several limitations. Firstly, our sample size was small and limited to only one out of the three residency programmes available in Singapore. Further studies are needed to ascertain if our findings are generalizable to other internal medicine programmes. Secondly, because the identities of residents were not tagged due to consent issues, our study could only capture the cohort effect as opposed to individual changes over time. In spite of that, our study provided interesting and novel insights that pave the way for future studies to employ the STF to further examine subspecialty choice for other senior residency programmes beyond internal medicine.
In summary, our study demonstrated that the factors that affect a resident’s choice of senior residency change over the years. As they mature, individual factors appear to exert a greater influence on their readiness to commit rather than contextual factors. Our pilot study suggests that the STF framework is a useful tool for career counselling for our residents that ought to start as early as year 1 of residency. Future studies should include a bigger sample size with tagged follow-ups to validate the use and effectiveness of the STF framework amongst our residents in Singapore.
Notes on Contributors
Joanne Kua is a consultant geriatrician in Tan Tock Seng Hospital, Singapore with a deep interest in medical education.
Mark Chan is a senior consultant geriatrician and Head of Department of the Department of Geriatric Medicine, Tan Tock Seng Hospital, Singapore.
Jolene See is a resident physician with the Department of Geriatric Medicine, Tan Tock Seng Hospital, Singapore.
David Ng is a senior resident in Geriatric Medicine with Tan Tock Seng Hospital, Singapore.
Lim Wee Shiong is a senior consultant geriatrician with Tan Tock Seng Hospital, Singapore and also an Adjunct Assistant Professor with the Yong Loo Lin School of Medicine.
Ethical Approval
Approval was obtained from the institutional review board of the National Healthcare Group.
Acknowledgements
We would like to acknowledge the NHG- AHPL residency programme for their help in making this study possible.
Declaration of Interest
Authors have no conflicts of interest, including no financial, consultant, institutional and other relationships that might lead to bias.
References
Aagaard, E. M., Dedier, J., & Julian, K. (2005). Factors affecting medical student’s selection of an internal medicine residency programme. Journal of the National Medical Association, 97(9), 1264- 1270.
Alexander, D. E., Osipow, S. H., & Savickas, M. L. (1985). Measuring Specialty Indecision among career decided students. Journal of Vocational Behaviour, 27, 356-367.
Chase, G. A., Levine, D. M., & Weisman, C. S. (1980). Male and female career patterns: Specialty choices and graduate training. Journal of Medical Education, 55, 813-825.
Chen, C. (2003). Integrating perspectives in career development theory and practice. The Career Development Quarterly, 51, 203-216.
Chibnall, J. T., Enoch, L., & Schindler, D. L. (2013). Association of medical student burnout with residency specialty choice. Medical Education, 47, 173-181.
Chou, H. Y., Hecker, R., & Martin, A. (2012). Predicting nurses well-being from job demands and resources: a cross-sectional study of emotional labour. Journal of Nursing Management, 20, 502-11.
Dorsey, E. R., Jarjoura, D., & Rutecki, G. W. (2003). Influence of controllable lifestyle on recent trends in specialty choice by US medical students. Journal of American Medical Association, 209(9), 1173- 1178.
Endler, P. C., Fuchs, S., & Messenholl-Strehler, E. (2011). Physician burnout in General Practitioners: Reflections upon prevention and treatment. International Journal of Communication, 5(2), 53-60.
Endler, P., Fischer, M., & Mitsche, M. (2013). Burnout in physiotherapists: Use of clinical supervision and desire for emotional closeness of distance to clients. International Journal of Therapy and Rehabilitation, 20(11), 550- 558.
Gillespie, D. F., Kalliath, T. J., & O’Driscoll, M.P. (2000). A test of the Maslach Burnout Inventory in three samples of healthcare professionals. Work and Stress, 14, 35-50.
Herr, E. L. (1997). Perspectives on career guidance and counseling in the 21st century. International Journal for Educational and vocational guidance, 50, 1-15.
Holden, W. D., & Levit, E. J. (1978). Migration of physicians from one specialty to another. Journal of American Medical Association, 239, 226-231.
Huggan, P. J., Samarasekara, D. D., & Ooi, S. B. S. (2012). The successful, rapid transition to a new model of graduate medical education in Singapore. Academic Medicine, 87, 1268-1273.
Jackson, J. R., Nuthalapaty, & F. S., Owen, J. (2004). The influence of quality of life, academic and workplace factors on residency programme selection. Academic Medicine, 79(5), 417-425.
Kontosh, L. G., & Zimmerman, A. L. (2007). A systems theory approach to career decision-making. Work, 29, 287-293.
Maslach, C., Jackson, S. E., & Leiter, M. P. (1996). Maslach Burnout Inventory (Third Edition). Palo Alto, California: Consulting Psychologists Press.
Osipow, S. H. (1999). Assessing career indecision. Journal of Vocational Behaviour, 55, 147-154.
Patton, W., & McMahon, M. (1999). Career development and systems theory: A new relationship. Pacific Grove, CA: Brooks/ Cole.
Patton, W., & McMahon, M. (2006). The systems theory framework of career development and counselling: connecting theory and practice. International Journal for the Advancement of Counselling, 28(2), 153-166.
Patton, W., & McMahon, M. (2014). Career development and systems theory: Connecting theory and practice. Holland. Rotterdam: Sense Publishers.
Redman, S., Saltman, D., & Straton, J. (1994). Determinants of career choices among women and men medical students and interns. Medical Education, 28, 361-371.
Richard, G. V., Savickas, M. L., Early, L., Calli, J., Englert, C. A. & Bono, J. (2007). Manual for the Specialty indecision Scale. District of Columbia, Washington, D.C.: Association of American Medical Colleges.
Samarasekara, D. D., Ooi, S., & Hooi, S. C. (2015). Medical education in Singapore. Medical Teacher, 37, 707-713.
*Kua Ee Chia Joanne
Address: 11 Jalan Tan Tock Seng Department of Geriatric Medicine Annex 2 Level 3
Tel: 63596474
Email: joanne_kua@ttsh.com.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









