Evaluation of a developmental paediatrics teaching programme for medical students
Published online: 7 May, TAPS 2019, 4(2), 25-31
DOI: https://doi.org/10.29060/TAPS.2019-4-2/OA2072
Yeleswarapu S. Padmini, Pratibha K. Agarwal & Lourdes M. Daniel
Department of Child Development, KK Women’s and Children’s Hospital (KKH), Singapore
Abstract
Introduction: The aim of the study was to evaluate the efficacy of the developmental paediatrics teaching programme for undergraduate medical students posted to the Department of Child Development (DCD), in a tertiary children’s hospital in Singapore.
Methods: Efficacy of the teaching program was evaluated objectively using multiple-choice questions (MCQs) and subjectively using a self-assessment evaluation form developed in-house. Feedback was obtained from the students and tutors at the end of the posting.
Results: 36 students participated in this evaluation. There was a significant positive difference in the pre and end of posting MCQ scores (p < 0.001). The difference in the students’ self-assessment of their knowledge and skills of child development before and at the end of their DCD posting was similarly positively significant (p < 0.001). Feedback from the students using a series of open-ended questions indicated that they had a very positive learning experience and this included learning beyond their stated learning objectives. Feedback from the tutors was reflective of some of the challenges they faced while teaching.
Conclusion: The integrated approach to teaching developmental paediatrics that includes didactic, reflective, interactive and problem-based learning results in a highly positive learning experience and enhances both the knowledge and skills in child development. This enables delivery of a holistic curriculum that goes beyond teaching mainly routine developmental assessment.
Keywords: Developmental Assessment, Developmental Paediatrics, Problem-based learning, Didactic Teaching, Medical Students
Practice Highlights
- Teaching medical students Developmental Assessment should not be limited to teaching them to conduct developmental assessment. They should be able to analyse child development in the context of impact on the functional ability in the child.
- Students should have the opportunity of engaging with not only families of neurotypical children, but those with disabilities, for them to understand the impact on the family.
- For the tutors, there is greater value in using various modalities of teaching approaches when teaching developmental paediatrics.
- Teaching can be incorporated within busy clinics through reflective learning.
I. INTRODUCTION
Increasing numbers of children are being identified with developmental and/or behaviour problems (Centers for Disease Control and Prevention, 2018). This is partly due to increased awareness of both the parents and clinicians, as well as increased survival of children born prematurely with complex medical conditions (Boyle et al., 2012). Primary care physicians are tasked with early identification of children with developmental delays/disorders during routine or opportunistic health surveillance consults. Decades of rigorous research indicates that early identification of developmental delays and timely early intervention can positively alter the child’s long term developmental trajectory (Oberklaid, Wake, Harris, Hesketh, & Wright, 2002; Scherzer, Chhagan, Kauchali, & Susser, 2012; Shevell, Majnemer, Platt, Webster, & Birnbaum, 2005). There is, however, evidence to suggest gaps in the knowledge and confidence of primary care providers in identifying and managing children presenting with developmental delays (Hastings, Lumeng, & Clark, 2014; Nicol, 2006). This could possibly be attributed to a lack of adequate training opportunities in child development during and after medical school (Nicol, 2006).
Medical education is constantly evolving to meet the demands of increasing numbers of students and changing emphasis on teaching and learning, with the eventual goal to improve patient care and satisfaction. The role of the educator, therefore, is to teach and guide a trainee/medical student to translate basic clinical knowledge into effective patient care. In the context of developmental paediatrics, medical students need to develop the knowledge and skills to take a comprehensive developmental history, identify developmental delays/disorders and develop clinical reasoning skills to evaluate further in terms of investigations and further management (Bellman, Byrne, & Sege, 2013). In addition, they should be able to understand the impact of the child’s disability on the child’s functioning as well as the impact on the family (Feyereislova & Nathan, 2014; Tracy & Graves, 1996). This holistic approach to patient management will enable young doctors of tomorrow to appreciate the critical role that families play in enhancing the developmental monitoring and support for their children. Most of the studies so far have evaluated teaching students to identify normal developmental milestones and conduct developmental screening using modalities such as didactic lectures and videos (Feyereislova & Nathan, 2014; Nicol, 2006). There is a paucity of studies addressing a more holistic developmental paediatric teaching programme for medical students.
With increasing emphasis on the clinicians to take on the role of educators, some of the challenges that the tutors face as clinical teachers include increasing student numbers, lack of adequate teaching opportunities in a busy clinic, tutor fatigue, difficulties recruiting patients for teaching purposes and lack of adequate training opportunities to prepare the tutors to be teachers (Frazer et al., 1999; Taylor, Tisdell, & Gusic, 2007). We developed a developmental paediatric teaching programme for the medical students, to provide a more holistic curriculum, delivered against the challenges faced including limited time and resources. The curriculum was based on the Paediatric Core Curriculum (PCC) which was designed by the expert PCC committee of the Lee Kong Chian (LKC) medical school. The modalities of delivery of the curriculum were decided after consultations with the experts within the Department of Child Development (DCD). The aim of the study was to evaluate the efficacy of the integrated teaching programme in enhancing the skills and knowledge of undergraduate medical students posted to the DCD. Skill areas included the ability to perform a developmental assessment (DA), to identify developmental delays and develop a management plan. Knowledge areas included knowledge of normal and abnormal patterns of development including aetiology and risk factors, management of a child presenting with developmental delay, awareness of the role of therapists and the range of community services available to the child and family.
II. METHODS
A. Site and Participants
The teaching programme was conducted at the DCD for fourth-year undergraduate medical students of LKC school of Medicine attached to the department from September 2016 to January 2017. The students were posted in three streams of four groups per stream, with four to five students per group for a total duration of eight half-day sessions. 36 medical students from streams one and two participated in the evaluation. As there was no funding for this project and due to constraints of resources in terms of time and manpower, the evaluation was limited to the two consecutive streams only.
B. Pre-posting Process
Information on learning objectives as prescribed in the LKC curriculum related to child development was made available to the medical students prior to their posting. Other reading materials included articles as outlined in the LKC curriculum such as assessment and management of developmental delays, learning difficulties, autism and ADHD. The students were also given a DA milestones chart that was developed in-house. All the tutors were sent the learning objectives and the DA milestones chart to ensure consistency of teaching practices.
C. Teaching Programme
The goal of our teaching programme was to produce competent students who had the required skills and knowledge for conducting appropriate DA, identify developmental delays and be aware of the management of the same as outlined in the LKC learning objectives. The students’ schedule was planned based on the learning objectives and resources available in terms of time, space and manpower. The posting started with an introductory session on child development. The students were allotted to clinics which included new cases and follow up cases. Each group had one to two ward-based sessions, one problem-based learning (PBL) session and they attended one observation of standardised developmental screening session. At the end of the posting, there was a debrief session with the LKC lead tutor for the DCD. On average the time spent on the various teaching components was approximately:
- Didactic lecture – 12%
- PBL – 12%
- Practical DA – 25%
- Observation of standardised developmental screening – 12%
- Reflective learning in clinic sessions – 34%
- Debrief session – 5%
D. Teaching Methodology
An integrated approach to teaching was adopted which included didactic (Luscombe & Montgomery, 2016), interactive learning (Feyereislova & Nathan, 2014), reflective learning (Sandars, 2009) and PBL (Preeti, Ashish, & Gosavi, 2013). All these strategies have been proven to be efficacious on their own in enhancing the learning of the trainees. Given the extent of the learning outcomes to be achieved, it was felt that the teaching methodology should incorporate all the above modalities of teaching. The introductory didactic lecture reviewed the developmental history, normal patterns of child development (0-5 years), factors affecting development and identification and management of developmental delays. It included videos to demonstrate how to conduct a DA. Some of the videos were developed in-house while others were obtained from various websites (Pathways, 2013).
During the clinic sessions, the students had opportunities to conduct DA on the index patient, on their typically developing siblings if accompanied and time permitted, learn various aspects of child development including identifying and management of developmental delays and disorders, and understand disability and its impact on the child and family. This was partly facilitated by observing clinician-parent interactions and reflective learning after each clinic session. The students were tasked with participating in patient evaluation by using various in-house developed screeners such as language and literacy screeners. There was a session with the assistant psychologists who routinely conduct developmental screening using Ages and Stages Questionnaires (ASQ-3) or Brigance III screener (Moodie et al., 2014) for all new cases referred to the DCD. This session provided the students with an opportunity to learn the use of developmental screeners. The ward-based sessions provided the medical students more hands-on opportunities to conduct DA on both neurotypical children, as well as children with developmental delays.
For the PBL session, the students were divided into two groups of two to three students and each group was given a clinical case vignette at the beginning of their DCD posting. Each case vignette was accompanied by learning objectives for the students to explore medical, physiological, anatomical and basic science concepts that relate to the clinical scenario. The students were expected to work in the groups for self-study and the final discussion was facilitated by one of the tutors. This provided with the opportunity for collaborative learning. The discussion included a holistic evaluation of the given case, starting from history taking to identification and management including approach towards the child and family.
A debrief session was conducted by the LKC lead tutor at the end of each group posting to obtain verbal feedback from the students using a series of open-ended questions regarding their experience of the DCD posting. The main aim of this session was to identify any potential gaps in the teaching that would enable us to modify the teaching programme for further groups. It was also another opportunity to answer any queries that the students may have in relation to any aspect of child development.
The students were asked the following questions:
- Did they feel that their learning outcomes were met, and if not why?
- Which sessions did they find useful and why?
- Which sessions did they not find useful and why?
- What aspect of the posting did they appreciate the most?
- Any further suggestions to enhance the learning opportunities for subsequent groups?
The responses were recorded on paper by the tutor. All the 36 students participated in the debrief sessions.
All the DCD LKC tutors were emailed to obtain feedback at the end of each stream posting. They were asked to state their experience of participating in teaching the medical students and identify the challenges they may have had if any. Only three out of the eight tutors responded back.
III. OUTCOME MEASURES
- Pre- and end of posting MCQs (n=10) included questions in relation to developmental milestones, screening tools for DA and red flags for delayed development. There were also case vignettes that covered the approach towards a child presenting with a developmental delay/ disorder.
- Self-assessment evaluation form with responses on a 5-point Likert scale ranging from 1 (poor) to 5 (excellent) to indicate knowledge and skills before and after the DCD posting. The knowledge and skills domain included 8 and 3 responses respectively (Table 1).
- Verbal feedback as obtained from the groups and written feedback from the tutors separately. No qualitative analysis of the same was conducted.
| Knowledge | ||||
| Pre | Post | Paired sample t-test | Significance (p value) | |
| Normal patterns of development | 2.1 ± 0.8 | 4.1 ± 0.5 | 13.5 | < 0.001 |
| Abnormal patterns of development | 1.8 ± 0.7 | 4.0 ± 0.7 | 16.3 | < 0.001 |
| Aetiology and risk factors for developmental delays | 1.8 ± 0.8 | 3.8 ± 0.7 | 13.9 | < 0.001 |
| Routine developmental assessment and new-born screening | 1.9 ± 0.9 | 4.0 ± 0.9 | 11.2 | < 0.001 |
| Screening tools to identify developmental delays | 1.6 ± 0.7 | 3.9 ± 0.7 | 15.0 | < 0.001 |
| Management of a child presenting with developmental delays | 1.5 ± 0.7 | 3.7 ± 0.7 | 17.7 | < 0.001 |
| Role of individual therapists in the management of a child presenting with developmental delay | 1.8 ± 0.9 | 3.8 ± 0.9 | 15.7 | < 0.001 |
| Awareness on range of services for pre-schoolers with developmental delays | 1.3 ± 0.6 | 3.8 ± 0.7 | 20.2 | < 0.001 |
| Skill | ||||
| Perform a development assessment | 1.7 ± 0.7 | 4.0 ± 0.6 | 17.6 | < 0.001 |
| Be able to detect delayed milestones (either as “Single-domain Delay” or “Global Developmental Delay”) | 1.8 ± 0.8 | 4.0 ± 0.8 | 17.9 | < 0.001 |
| Developing a management plan for a child presenting with developmental delay | 1.4 ± 0.6 | 3.6 ± 0.7 | 17.7 | < 0.001 |
Table 1. Students’ self-assessment of knowledge between pre and end of the DCD posting (post)
IV. RESULTS
A. MCQs
There was a significant improvement in the overall score between the pre and end of posting MCQs with the scores improving from 7.0 ± s1.6 (pre-posting score) to 8.9 ± 0.9 (end of posting score), which was highly significant (p < 0.001) (Figure 1).
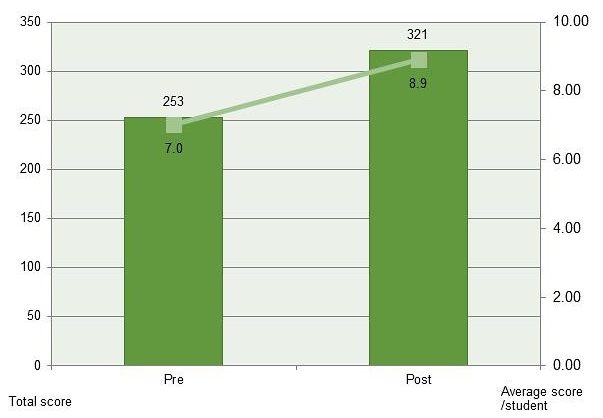
Figure 1. Pre and end of posting MCQs
Students reported a significant improvement in their self-assessment of knowledge and skills in relation to child development after the DCD posting and this was found to be statistically significant (Table 1). In the context of knowledge, the domain where the maximum positive change was noted was awareness of the range of services for pre-schoolers with developmental delays (paired t-test 20.2; p < 0.001) followed by management of a child presenting with developmental delays (paired t-test 17.7; p < 0.001). The domain of least change, albeit statistically significant was knowledge of routine developmental assessment and new-born screening (paired t-test 11.2; p < 0.001).
In the context of skills, all the three domains indicated a similar positive shift between the pre- and end of posting evaluation (p < 0.001).
B. Student Feedback
The feedback from the students was positive overall. In relation to the specific questions that were asked, the summary of the responses is as below.
1) Did they feel that their learning outcomes were met, and if not why? All the thirty-six students commented that their learning outcomes were met. In fact, they learnt well and above their stated learning objectives. Some comments included:
“I understand the liaison that’s needed with the various agencies working with the child and family, be it in the school, hospital or community.”
“I now understand the social and financial implications of having a child with developmental delay.”
2) What sessions they found useful and why? All the thirty-six students reported that they found new case clinics and ward-based sessions most useful as they had more opportunities to practise DA. In addition, some students reported that they liked the PBL session as this session helped them understand a case more holistically. Some comments included:
“Ward-based sessions helped understand development in typically developing children, while clinic sessions helped identify children with developmental delays and disorders.”
“PBL session was very useful. It forced us to ‘do our homework’. Brought us back to the basics. It helped to consolidate what we have learnt during the posting so far.”
3) What sessions that they did not find useful? Some students felt that they did not have adequate learning opportunities during busy follow-up clinic sessions.
4) What aspect of the posting do they appreciate the most? While some students commented that they appreciated the approachability and teaching provided by the tutors in the DCD the most, others commented that it was the social aspects of the various conditions and learning how to support and counsel the family they appreciated the most. Some comments included.
“The tutors were very approachable and willing to teach in spite of a busy clinic.”
“Exploration of social concerns and counselling were very insightful.”
5) Any further suggestions to enhance the learning opportunities for subsequent groups? Some of the suggestions that came from them included scheduling the DA lecture at the beginning of the stream posting rather than at the start of the DCD posting. This would give the students the knowledge and skills to enable them to practise DA even when posted in the other paediatric departments. They requested for more ward-based tutorials and a longer DCD posting.
C. Tutor Feedback
Although all the tutors were willing to teach the students, some of the challenges that they reported included lack of adequate teaching opportunities during clinics, especially when the clinics were busy. Some of the tutors felt that the clinical sessions such as autism specialist clinics were too specialised and hence are not suitable for the students. The tutors also did not have the time to commit to ward-based sessions on a regular basis. During the sessions when two students were attached to a clinic, some tutors felt that this could overwhelm the child and family and could affect the child’s DA.
V. DISCUSSION
Our study confirms the significant benefits of and enhancement of positive learning outcomes using an integrated approach of teaching developmental paediatrics to undergraduate medical students. The improvement covered a broad range of areas including knowledge of normal and abnormal developmental patterns, management of a child presenting with developmental delays, awareness of the range of services for such children and skills to conduct a DA and formulate a management plan for a child with developmental delay. These are the essential skills required of any practitioner working with children. The students had exposure to neurotypical children as well as to children with disabilities and their families during the posting. This helped them appreciate normal from abnormal patterns of development, as well as the social impact of the disability on the child and family. The end of posting feedback from the students reflected the learning of the students beyond the prescribed learning outcomes during the posting. Despite the challenges mentioned in the tutors’ feedback, their intent in teaching DA effectively and being able to provide a conducive teaching environment was evident from the positive feedback reported by the students and from the outcome measures.
It is being increasingly recognised that teaching developmental paediatrics should be holistic, and incorporate all the aspects of child development (McDonald, 2018; Tracy & Graves, 1996). While it is imperative that the students are familiar with the developmental milestones and how to elicit them, it is equally important for them to understand the functional aspects of the child’s developmental milestones. This will enable them to give appropriate anticipatory guidance to the parents/carers. It is also essential that the students are able to appreciate the functional impact of the child’s delays/disability on both the child and the family. This knowledge will enable to help them learn to counsel the parents appropriately. Teaching through exposure to children with special needs and their families will significantly improve knowledge and skills of the medical students (McDonald, 2018; Ryan & Scior, 2014; Whitehall, McCulloch, Edwards, & McDonald, 2015).
VI. LIMITATIONS OF THE STUDY
While some of the teaching sessions were structured, others that involved teaching within the clinics were unstructured and hence the students were exposed to various teaching modalities within these clinical sessions. At times during busy clinics, teaching the students could have been compromised, although they would still have had the opportunity to learn from clinician-parent/patient interactions. Although feedback was obtained from the students and tutors after the posting, qualitative evaluation of the same was not conducted. Less than 50% of the tutors responded back, hence the tutor feedback as stated above is not completely reflective of their experiences including challenges in teaching the students. The teaching curriculum was delivered through various modalities, which could not be individually evaluated in terms of the efficacy of each one of them separately. Functional aspects of child developmental milestones, which is a very important component of child development were discussed by the more experienced tutors during various sessions, but this was not evaluated. The student’s knowledge of developmental paediatrics was assessed through MCQs and no formal evaluation of skills was conducted in view of the short duration of the DCD posting. While we are encouraged by the positive results of our educational model, we would also acknowledge that we did not aim to demonstrate its superiority over other educational models as there was no such direct comparison in our study. Further research into comparing various educational models need to be explored.
VII. CONCLUSION
The teaching programme developed by the department was deemed to very effective by the undergraduate medical students, in enhancing their knowledge and skill in developmental paediatrics. Increasing student numbers would require teaching methodologies to constantly evolve, without having an impact on the quality of teaching or clinical care. While the above methodology of curriculum has worked well for smaller group setting, it may have to be modified as the numbers increase.
Notes on Contributors
Dr Padmini Yeleswarapu is a Senior Clinical Lecturer, Yong Loo Lin School of Medicine (YLLSoM), Adjunct Assistant Professor, Duke-NUS Graduate Medical School and is working as a Consultant Paediatrician, Department of Child Development, KK Women’s and Children’s Hospital. She is also a Clinical Teacher in Lee Kong Chian School of Medicine (LKCSoM).
Dr Pratibha Agarwal is a Senior Consultant in the Department of Child Development, KKH. She was a Senior Clinical Lecturer in YLL-NUS School of Medicine from 2009 to 2014, an Adjunct Assistant Professor in Duke-NUS from 2010 to 2014 and currently a Clinical Teacher in Lee Kong Chian School of Medicine (LKCSoM).
A/Prof Mary Daniel is the Senior Consultant and Head of Department of Child Development, KKH. She is an Adjunct Associate Professor of Duke-NUS, YLLSoM and LKCSoM; is a reviewer for the Annals of the Academy of Medicine, Singapore and on the Editorial Board of Journal of Clinical Pathology and Diagnosis.
Ethical Approval
Ethical approval was sought from the Institutional Review Board (IRB) and was deemed not necessary.
Acknowledgements
We would like to thank the medical students who participated in the study and Ang Cheng Hiang and Lek Evelyn for their support and help in data management.
Funding
The research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of Interest
The authors warrant that the article is original, does not infringe upon any copyright or other proprietary right of any third party, is not under consideration by another journal and has not been previously published. Authors have no conflicts of interest, including financial, institutional and other relationships that might lead to bias.
References
Bellman, M., Byrne, O., & Sege, R. (2013). Developmental assessment of children. British Medical Journal, 346, e8687. https://doi.org/10.1136/bmj.e8687
Boyle, E. M., Poulsen, G., Field, D. J., Kurinczuk, J. J., Wolke, D., Alfirevic, Z., & Quigley, M. A. (2012). Effects of gestational age at birth on health outcomes at 3 and 5 years of age: Population based cohort study. British Medical Journal, 344, e896. https://doi.org/10.1136/bmj.e896
Centers for Disease Control and Prevention, National Center for Health Statistics. (2018, April 9). Key findings: Trends in the prevalence of developmental disabilities in U. S. children, 1997–2008 [Webpage]. Retrieved from
https://www.cdc.gov/nchs/ppt/nchs2012/ss-22_blumberg.pdf
Feyereislova, S., & Nathan, D. (2014). How best to teach developmental assessment? A single-blinded randomised study. Archives of Disease in Childhood, 99(12), 1083-1086. https://doi.org/10.1136/archdischild-2013-305536
Frazer, C., Emans, S. J., Goodman, E., Luoni, M., Bravender, T., & Knight, J. (1999). Teaching residents about development and behavior: Meeting the new challenge. Archives of Pediatrics and Adolescent Medicine, 153(11), 1190-1194.
https://doi.org/10.1001/archpedi.153.11.1190
Hastings, E. A., Lumeng, J. C., & Clark, S. J. (2014). Primary care physicians’ knowledge of and confidence in their referrals for special education services in 3- to 5-year-old children. Clinical Pediatrics, 53(2), 166-172.
https://doi.org/10.1177/0009922813503036
Luscombe, C., & Montgomery, J. (2016). Exploring medical student learning in the large group teaching environment: Examining current practice to inform curricular development. BioMed Central Medical Education, 16(1), 184.
https://doi.org/10.1186/s12909-016-0698-x
McDonald, J. (2018). Twelve tips for teaching child development and disability to medical students. Medical Teacher, 40(2), 135-139. https://doi.org/10.1080/0142159X.2017.1365118
Moodie, S., Daneri, P., Goldhagen, S., Halle, T., Green, K., & LaMonte, L. (2014). Early childhood developmental screening: A compendium of measures for children ages birth to five. Retrieved from Administration for Children and Families, U.S. Department of Health and Human Services Website:
https://www.acf.hhs.gov/sites/default/files/opre/compendium_2013_508_compliant_final_2_5_2014.pdf
Nicol, P. (2006). Using the ages and stages questionnaire to teach medical students developmental assessment: A descriptive analysis. BioMed Central Medical Education, 6(1), 29. https://doi.org/10.1186/1472-6920-6-29
Oberklaid, F., Wake, M., Harris, C., Hesketh, K., & Wright, M. (2002). Child health screening and surveillance: A critical review of the evidence. Retrieved from
http://www.esdy.edu.gr/files/011_Ygeias_Paidiou/Koinonikh_Paidiatrikh_tei_mathimata/A6_Paidia_Screening_Australia_2002.pdf
Pathways [Screen name]. (2013, February 6). 6 month old baby typical and atypical development [Video file]. Retrieved from https://www.youtube.com/watch?v=sUO6baJ0FcA
Preeti, B., Ashish, A., & Gosavi, S. (2013). Problem based learning (PBL) – An effective approach to improve learning outcomes in medical teaching. Journal of Clinical and Diagnostic Research, 7(12), 2896-2897. https://doi.org/10.7860/JCDR/2013/7339.3787
Ryan, T. A., & Scior, K. (2014). Medical students’ attitudes towards people with intellectual disabilities: Literature review. Research Developmental Disabilities, 35(10), 2316-2328. https://doi.org/10.1016/j.ridd.2014.05.019
Sandars, J. (2009). The use of reflection in medical education: AMEE guide no. 44. Medical Teacher, 31(8), 685-695. https://doi.org/10.1080/01421590903050374
Scherzer, A. L., Chhagan, M., Kauchali, S., & Susser, E. (2012). Global perspective on early diagnosis and intervention for children with developmental delays and disabilities. Developmental Medicine and Child Neurology, 54(12), 1079-1084. https://doi.org/10.1111/j.1469-8749.2012.04348.x
Shevell, M., Majnemer, A., Platt, R. W., Webster, R., & Birnbaum, R. (2005). Developmental and functional outcomes at school age of preschool children with global developmental delay. Journal of Child Neurology, 20(8), 648-653.
https://doi.org/10.1177/08830738050200080301
Taylor, E. W., Tisdell, E. J., & Gusic, M. E. (2007). Teaching beliefs of medical educators: Perspectives on clinical teaching in paediatrics. Medical Teacher, 29(4), 371-376.
https://doi.org/10.1080/01421590701510553
Tracy, J., & Graves, P. (1996). Medical students and people with disabilities: A teaching unit for medical students exploring the impact of disability on the individual and the family. Medical Teacher, 18(2), 119-124.
https://doi.org/10.3109/01421599609034145
Whitehall, J., McCulloch, R., Edwards, M., & McDonald, J. (2015). Engagement of undergraduate medical students of paediatrics in special schools for children with disabilities. Journal of Paediatrics and Child Health, 51(8), 798-801.
https://doi.org/10.1111/jpc.12831
*Yeleswarapu Sita Padmini
Department of Child Development,
KK Women’s and Children’s Hospital
100 Bukit Timah Rd,
Women’s Tower, Level 5,
Singapore 229899
Email: yeleswarapu.padmini@singhealth.com.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









