I. How do tubulointerstitial diseases present clinically?
1. Polyuria, nocturia
2. Signs and symptoms of infection (pyelonephritis) - fever, flank pain and tenderness, urinary frequency, bacteraemia, pyuria
3. Severe renal colic (spasmodic pain) and haematuria - this occurs in nephrolithiasis (stones in the kidney)
4. Acute renal failure (seen in Acute Interstitial.Tubulointerstitial Nephritis and Acute Tubular Necrosis - below)
Oligura /Anuria (marked decrease or absence of urine production)
Azotaemia (progressive rise in serum creatinine)
II. What are some tubulointerstitial diseases according to the main aetiologic categories?
1. Inflammatory conditions
i. Acute interstitial.tubulointerstitial nephritis (AIN)
Causes:
Drugs (eg. NSAIDs, antibiotics)
Autoimmune disease
Non-kidney infections
Clinical presentation: Acute renal failure
2. Acute pyelonephritis
Causes:
Infectious agents - Bacterial, from ascending infections (vesico-ureteric reflux, calculi, tumous, exacerbated by Diabetes)
Less commonly from haematogenous soread
Clinical presentation: Fever, flank pain, urinary symptoms, acute renal failure
3. Chronic pyelonephritis
Definition: Chronic and progressive renal scarring with involvement of calyces and pelvis
Causes: Infections - Vesicoureteric reflux, calculi, obstruction
Complicationx: Chronic renal failure
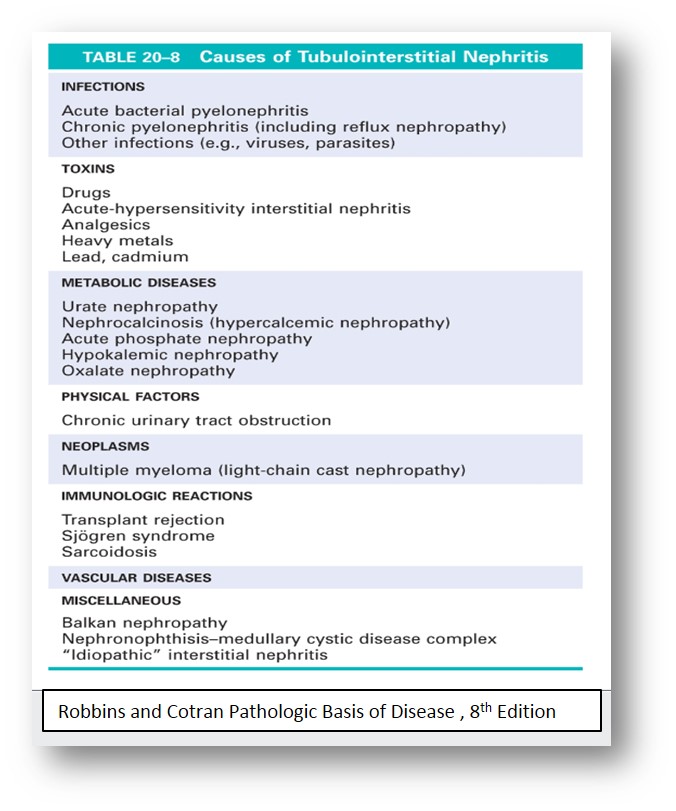
This chart, taken from Robbins, describes the many possible causes of tubular diseases. The commonest causes fall into 3 categories: Toxic, ischaemic and infectious.
Many kidney diseases have secondary effects of the renal vessels.
In addition, many systemic conditions also cause changes in the renal vessels. You can find a good discussion of these in the Kidney chapter in Robbins and Cotrans Pathologic Basis of Disease.
Here are a few important conditions that affect the renal vessels:
1. Hypertension
Benign nephrosclerosis - This refers to the renal pathology associated with sclerosis of the renal arteries and arterioles, as very often seen in hypertension
- Vascular changes - hyaline arteriolosclerosis (small arteries and arterioles); fibroelastic hyperplasia (interlobular and arcuate arteries)
- Renal parenchyma - Ischaemic changes à Glomerular collapse and fibrosis, tubular atrophy
- Gross findings: Subcapsular scars, mildly shrunken kidney
- Functionally, kidneys usually still maintain fairly good renal function but may progress to renal failure, especially if they have concomitant diabetes
Malignant nephrosclerosis - Seen in malignant hypertension (systolic BP > 200mmHg, diastolic > 120mmHg)
- Vessels - Fibrinoid necrosis (arterioles, glomeruli) , hyperplastic arteriolosclerosis (interlobular arteries and arterioles - onion-skin appearance; may have superimposed thrombosis)
- Kidney parenchyma becomes ischaemic and there is activation of the renin-angiotensin system, may show petechial haemorrhages from ruptured arterioles and glomeruli
- Clinically: renal failure, hypertensive encephalopathy with signs and symptoms of raised ICP, heart failure
2. Diabetes
Vascular changes similar to those seen in benign nephrosclerosis can be seen, in addition to tubular changes and specific glomerular changes (eg. nodular appearance of the mesangium, Kimmelstiel-Wilsom nodules). Specific changes are described in your lecture notes.
3. Amyloidosis
This is usually seen in plasma cell dyscracias and chronic inflammatory disease states when there is kidney involvement. There are extracellular Congo Red-positive fibrillart amyloid deposits in the glomeruli, interstitium and vessels. Note that this condition affects multiple compartments of the renal parenchyma, similar to diabetes.
There are other conditions involving the renal vessels, eg. renal artery stenosis, renal infarction (most are due to emboli from the heart or aorta) and vasculitic diseases, which you can read more about in your textbooks.
- Home
- Pathology Demystified
- Urogenital Pathology
- Tubulointerstitial and Vascular Diseases