Hi students, here is an example of a real life case that is handled by a pathologist in the diagnostic pathology laboratory.
This is a COLONIC TUMOUR from a right hemicolectomy specimen that is received from the operating theatre.
The pathologist's role is to provide diagnostic and prognostic information for the managing team (surgeons, medical and radiation oncologists etc).
Let's walk through this case from the beginning:
I. History and relevant investigations
Mr Tan, a 77 year old retired taxi driver, presents with lower abdominal pain and loss of weight over the past 3 months. He had a faecal occult blood test which was negative.
(Click HERE to find out more about faecal occult blood test as a screening tool for colorectal cancer in Singapore.)
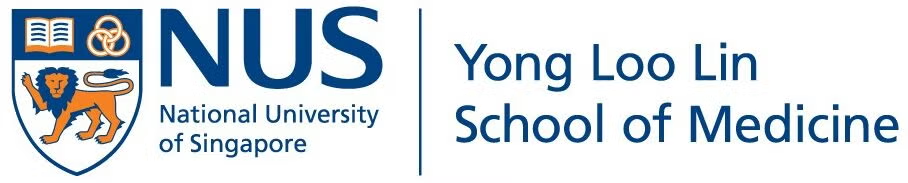
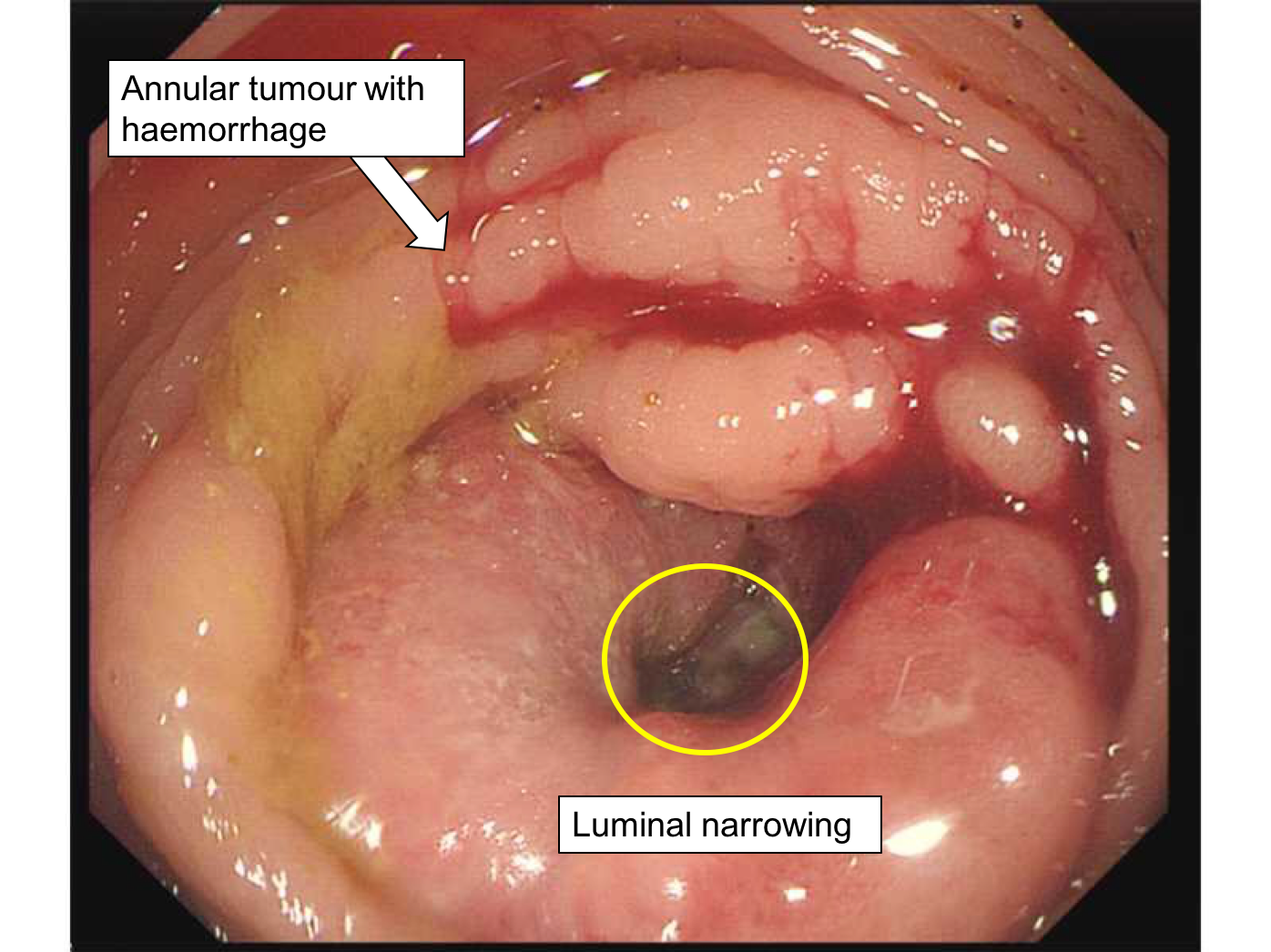
Colonoscopy was performed:
Staging investigations included CT scan of the thorax, abdomen and pelvis which showed no other tumour deposits.
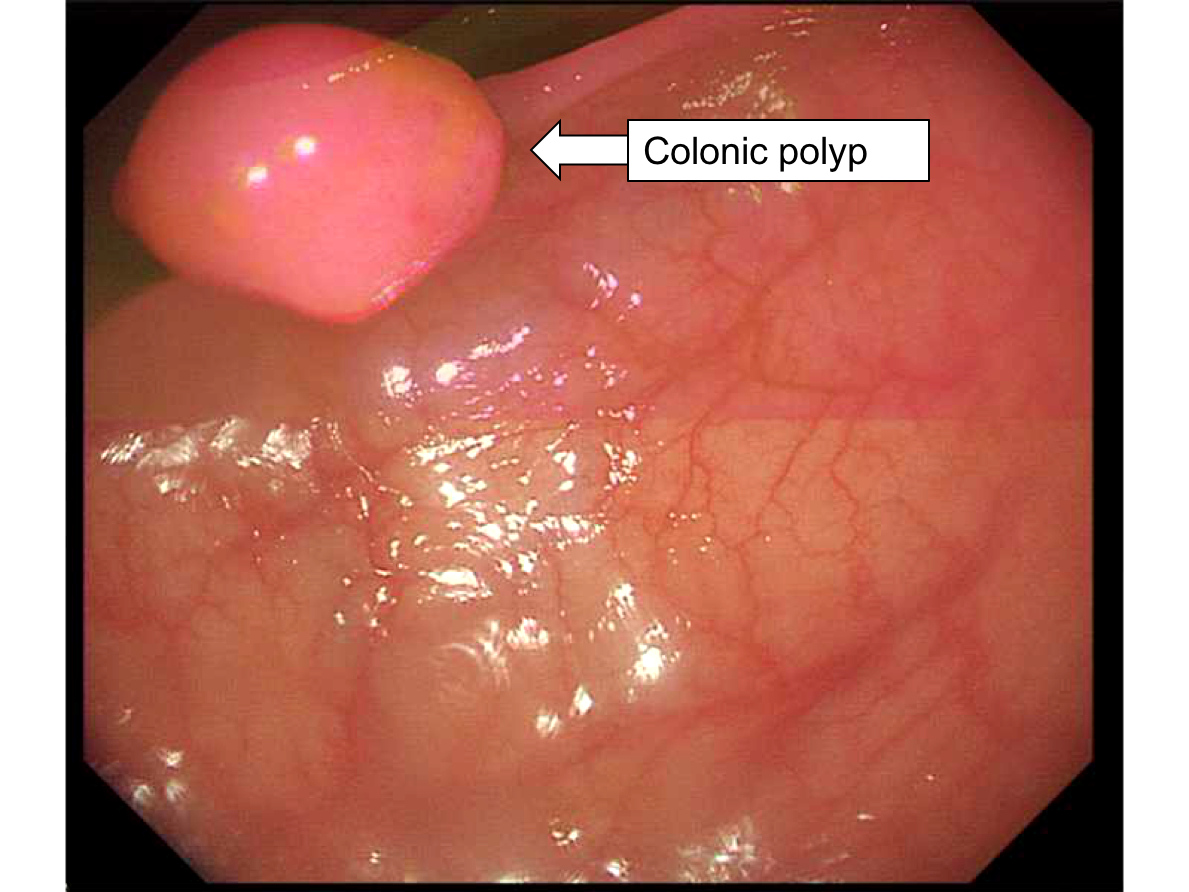
His baseline serum CEA was 41ug/L. CEA is a tumour marker for colorectal cancer and can be used to monitor response to therapy and disease recurrence.
Mr Tan underwent an extended right hemicolectomy and the specimen was sent to the pathology lab.
II. In the Pathology Lab
Upon receiving the specimen, the first step is to describe it and sample relevant tissues for microscopic examination. This is called "Grossing".
Video 1. Grossing the colon
If you can't play the video, watch it here on YouTube: https://youtu.be/mTuVNMDcqIo
The sampled sections and then processed into sections on glass slides.The pathologist examines them.
Video 2. Microscopic examination
If you can't play the video, watch it here on YouTube: https://youtu.be/S9hdY_gSx7k
III. Final Pathology Report
The pathologist then writes a report of his/her findings, which is conveyed to the managing team
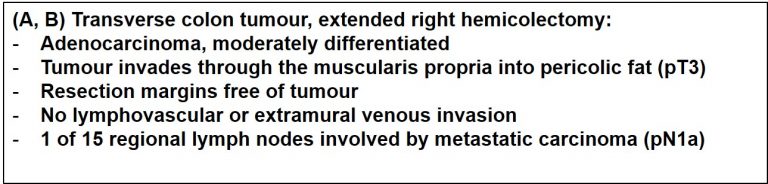
According to the TNM staging for colorectal cancer, pT3 N1a M0 belongs to the cancer stage group IIIB. The prefix "p" represents pathological staging (on microscopic examination).
IV. Post-operative care and beyond
Mr Tan had an uncomplicated post-operative recovery and was discharged from hospital 6 days after the surgery.
His case was discussed at a multi-disciplinary team meeting (Colorectal Oncology Tumour Group). This is a weekly meeting attended by surgeons, oncologists, pathologists, radiologists, nurse consultants and allied health professionals involved in the care of patients with colorectal cancer.
The consensus was that Mr Tan should have post-operative chemotherapy, as it has been shown in clinical trials to offer survival benefit in patients with a similar stage of cancer.
Mr Tan was seen at the oncology outpatient clinic 1 month after the operation, where he decided not to have chemotherapy. He will have follow-up CT scans and his serum CEA level will be monitored according to local protocols.
This case demonstration was jointly created by Dr Seet Ju Ee, and Dr Noel Chia Department of Pathology, National University Hospital, Singapore.