Mild Cognitive Impairment (MCI) vs Healthy Ageing Brain

Mild Cognitive Impairment (MCI) has been positioned as the intermediate stage between normal ageing and dementia. People with MCI experience some decline in their memory or thinking processes, but the symptoms are less severe than that of dementia. Early detection of cognitive decline is of utmost importance as better management is dependent on early adequate care and prevention measures (Liu et al., 2022).
As we age, it is natural to experience changes in our cognitive ability. Past research have found that working memory and short-term recall gradually decline with ageing. In addition, people also experience a decline in information processing speed, explaining why it is harder for older folks to learn new things (Yankner et al., 2008).
So, what is the line that separates normal ageing and MCI?
The Healthy Ageing Brain
Ageing causes changes in brain size, vasculature, and cognition. Losing some cognitive ability is a completely natural part of ageing (Liu et al., 2022). While different cognitive function peaks at different ages, it is generally accepted that a person’s cognitive prowess follows an inverted U trend (Cai et al., 2014).
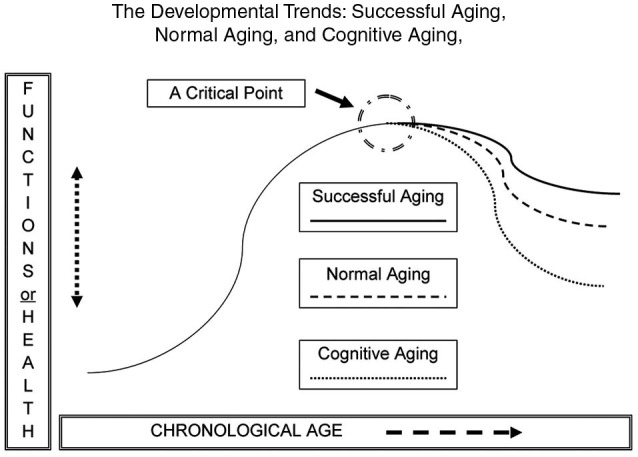
Picture from Cai et al., 2014
As you might have observed or experienced personally, the most common declines include:
- Decreased information processing speed
- Declined working memory
- Declining attention span
- Difficulty multitasking
That is not to say that all cognitive abilities decline with age. Some research have suggested that vocabulary, verbal knowledge, emotional stability and the ability to evaluate other people’s emotions remain the same or even improve along with age (Yankner et al., 2008).
What is Mild Cognitive Impairment (MCI)?
While subtle changes are expected, some people experience a decline that is more than what would be considered normal. The symptoms of MCI are not as severe as dementia and most people with MCI are able to live independently. Early signs of MCI include:
- Forgetfulness & memory lapse
- Impaired sense of direction
- Changes in personality or mood
- Language problems
- Disorientation in time
It is important to note that what is normal for one person might not be the case for another. What is considered “normal” is relative to the person’s age, education, employment status, and overall living environment.
MCI has a prevalence of 12.5% in Singapore. Gender is found to be significantly associated with MCI subtypes, with males more likely to have aMCI (amnestic MCI) and females more likely to have naMCI (non-amnestic MCI) (Liu et al., 2022).
Types of Mild Cognitive Impairment
Symptoms could be classified into 2 types: amnestic and non-amnestic MCI. That is:
Amnestic MCI Symptoms
- Getting lost in familiar places
- Forgetting recent events or appointments
- Forgetting names or conversations
Non-amnestic MCI Symptoms
- Changes in personality and behaviours
- Change in diet/eating habit
- Decline in language ability (comprehension & verbal)
- Loss of balance
- Declining attention span
Managing MCI
Unfortunately, there is still no cure for cognitive decline. The risk of depression and anxiety is also higher in those with MCI as compared to the general population.
The research has since shifted towards non-pharmaceutical interventions to improve emotional states, enhance cognitive function, and delay or even reverse the symptoms of cognitive decline.
A healthy life both physically and mentally may be the best defence against the changes of an ageing brain.
World Alzheimer Report 2015 – The global impact of dementia: An analysis of prevalence, incidence, cost, and trends. Alzheimer’s Disease International (ADI).
Mind Science Centre’s Jurong Ageing Study (JAS)
JAS aims to explore the effects of preventive psychosocial interventions on older adults with MCI to examine its potential as an intervention method for cognitive decline. These interventions include:
- Health education programme (HEP)
- Mindfulness Awareness Practice (MAP)
- Therapeutic horticulture
- Art activities
- Tai chi exercise
- Music-reminiscence
- Choral singing
- Tea drinking
Our research showed evidence of improved cognitive function (Fam et al., 2020; Yu et al., 2021), gut bacteria profiles (Khine et al., 2020), telomere lengths (Yu et al., 2020), and inflammatory biomarkers (Ng, 2020) following the interventions. Click here for more details on Mind Science Centre’s Jurong Ageing Study.
Above that, these interventions are low-cost, self-directed, and can be practised without much time and space constraints, further suggesting its potential for success in Singapore communities.
Ageing with Dignity: Age Well Everyday (AWE) Programme
In addition to research, it is of our utmost interest to ensure that our research findings are translated into programmes that have a direct impact on the community. Our programmes seek to allow seniors to age with dignity and have a great quality of life for as long as possible.
In expanding the Jurong Ageing Study, we started the Age Well Everyday (AWE) Programme in which we recruited and trained seniors as volunteers to lead community activities and interventions mentioned above. AWE is special as the programme places emphasis on preventive medicine in the community, by the community, for the community.
We are proud to be in collaboration with 8 centres across the island, with further expansion plans coming along. Find out how you can join our AWE programme here.
References
Liu, L.-Y., Lu, Y., Shen, L., Li, C.-B., Yu, J.-T., Yuan, C. R., et al. (2022). Prevalence, risk and protective factors for mild cognitive impairment in a population-based study of Singaporean elderly. J. Psychiatr. Res. 145, 111–117. doi: 10.1016/j.jpsychires.2021.11.041
Yankner, B. A., Lu, T., & Loerch, P. (2008). The Aging Brain. Annual Review of Pathology: Mechanisms of Disease, 3(1), 41–66. https://doi.org/10.1146/annurev.pathmechdis.2.010506.092044
Cai, L., Chan, J. S. Y., Yan, J. H., & Peng, K. (2014). Brain plasticity and motor practice in cognitive aging. Frontiers in Aging Neuroscience, 6. https://doi.org/10.3389/fnagi.2014.00031
Prince, M, Wimo, A, Guerchet, M, Ali, GC, Wu, Y. T., and Prina M. World Alzheimer Report 2015 – The Global Impact of Dementia: An analysis of prevalence, incidence, cost and trends. London: Alzheimer’s Disease International (ADI); 2015.
Fam, J., Sun, Y., Qi, P., Lau, R. C., Feng, L., Kua, E. H., & Mahendran, R. (2020). Mindfulness practice alters brain connectivity in community‐living elders with mild cognitive impairment. Psychiatry and Clinical Neurosciences, 74(4), 257–262. https://doi.org/10.1111/pcn.12972
Yu, J., Rawtaer, I., Feng, L., Fam, J., Kumar, A. P., Kee-Mun Cheah, I., Honer, W. G., Su, W., Lee, Y. K., Tan, E. C., Kua, E. H., & Mahendran, R. (2021). Mindfulness intervention for mild cognitive impairment led to attention-related improvements and neuroplastic changes: Results from a 9-month randomized control trial. Journal of Psychiatric Research, 135, 203–211. https://doi.org/10.1016/j.jpsychires.2021.01.032
Khine, W. W. T., Voong, M. L., Ng, T. K. S., Feng, L., Rane, G. A., Kumar, A. P., Kua, E. H., Mahendran, R., Mahendran, R., & Lee, Y.-K. (2020). Mental awareness improved mild cognitive impairment and modulated gut microbiome. Aging, 12(23), 24371–24393. https://doi.org/10.18632/aging.202277
Yu, J., Kanchi, M. M., Rawtaer, I., Feng, L., Kumar, A. P., Kua, E.-H., & Mahendran, R. (2020). The functional and structural connectomes of telomere length and their association with cognition in mild cognitive impairment. Cortex, 132, 29–40. https://doi.org/10.1016/j.cortex.2020.08.006
Ng, T. K. S., Fam, J., Feng, L., Cheah, I. K.-M., Tan, C. T.-Y., Nur, F., Wee, S. T., Goh, L. G., Chow, W. L., Ho, R. C.-M., Kua, E. H., Larbi, A., & Mahendran, R. (2020). Mindfulness improves inflammatory biomarker levels in older adults with mild cognitive impairment: a randomized controlled trial. Translational Psychiatry, 10(1). https://doi.org/10.1038/s41398-020-0696-y